The Alveolar Bone Provides Support to Teeth and Other Functions: A Review
Michel Goldberg1*
1Department of Oral Biology, Faculty of Fundamental and Biomedical Sciences, INSERM UMR-S 1124 Paris Cite University, France
*Corresponding Author: Michel Goldberg, Department of Oral Biology, Faculty of Fundamental and Biomedical Sciences, INSERM UMR-S 1124 Paris Cite University, France; Email: [email protected]
Published Date: 04-03-2022
Copyright© 2022 by Goldberg M. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 03 Feb, 2022 | Accepted 25 Feb, 2022 | Published 04 Mar, 2022 |
Abstract
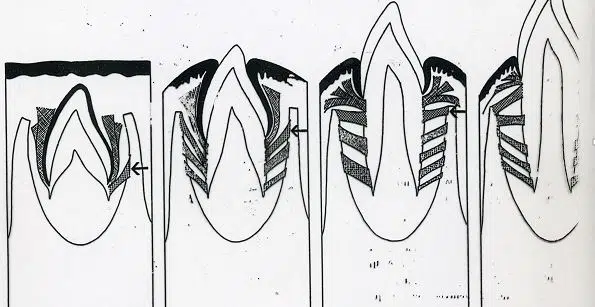
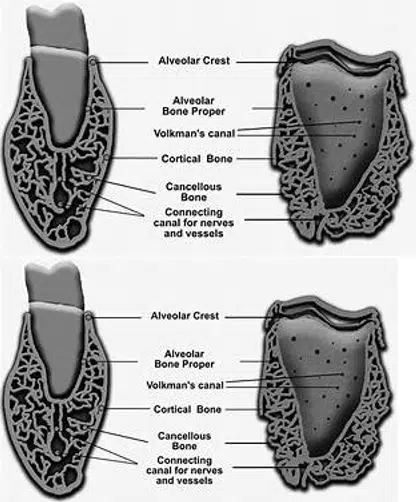
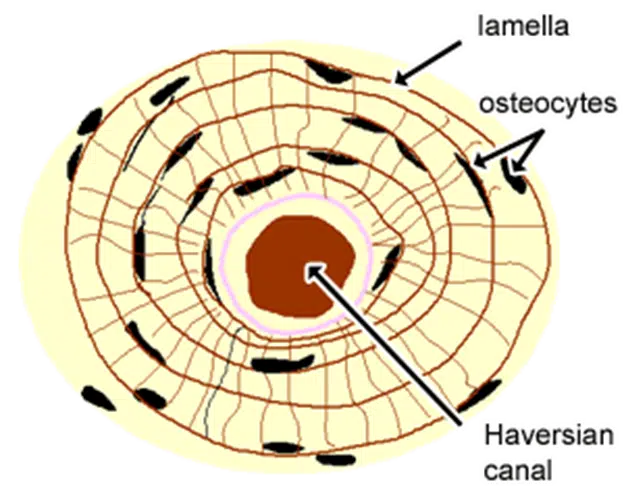
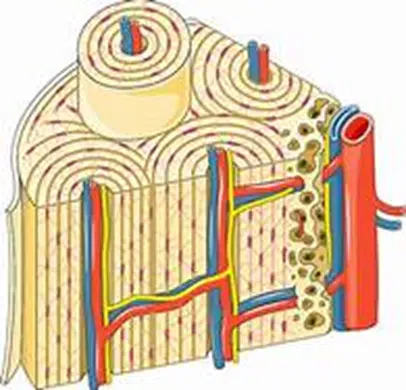
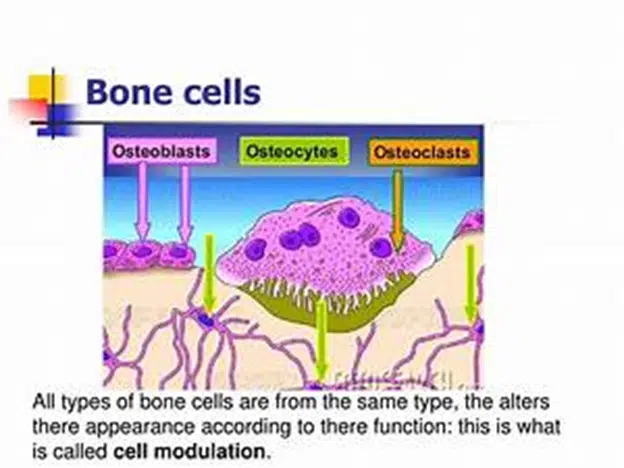
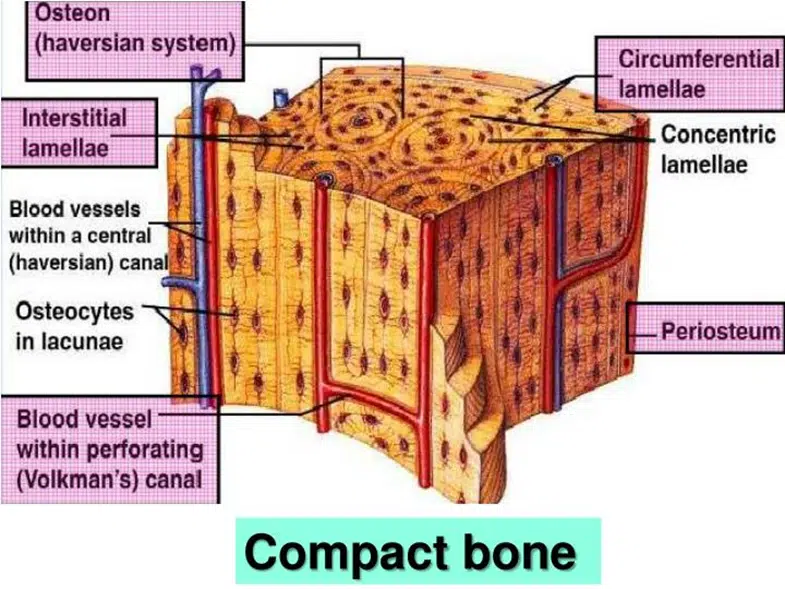
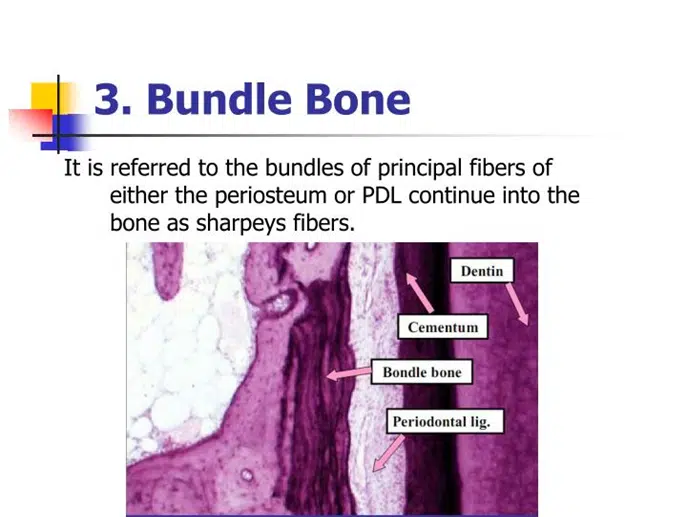
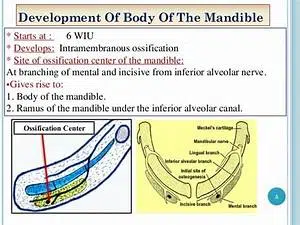
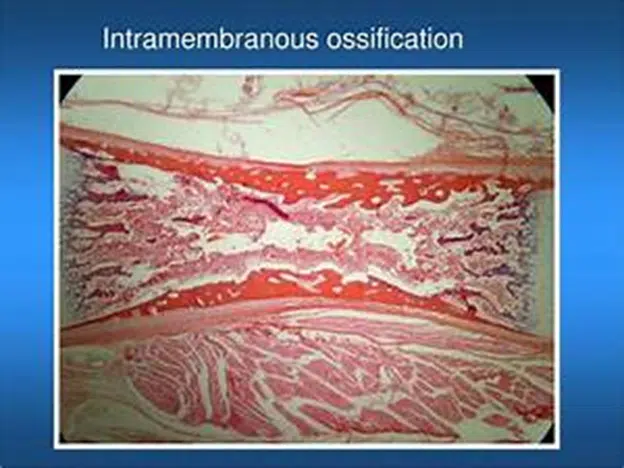
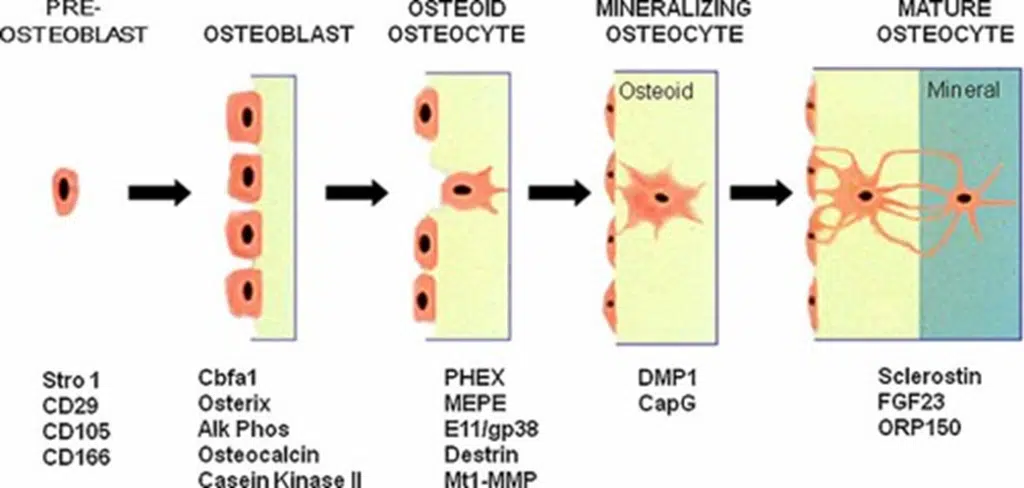
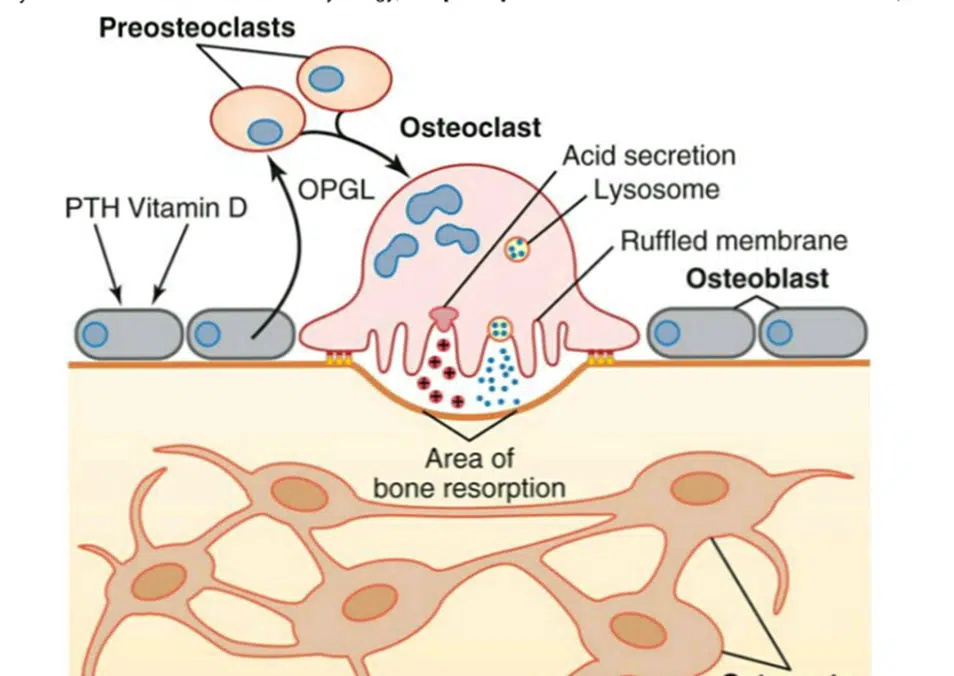
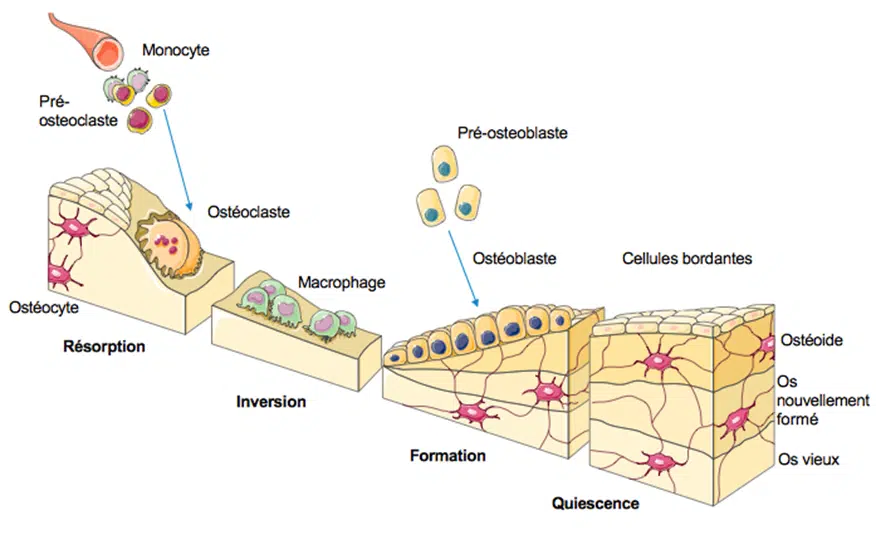
Alveolar bone provides structural supports to teeth. The outer and inner compact bone are formed by osteons, the basic structure of cortical bone, with a central vertical Haversian canal and rings forming a lamellar bone (bundle or alveolar bone). The central cancellous bone is the spongiosa (spongy bone). Bundles of collagen fibers (Sharpey’s fibers) provide attachment of the root to bone. Perforating Volkmann’s canals, limiting the inner bone are forming “the cribliform plate”. Oriented horizontally, the plate contains blood vessels and nerves issued from the periosteum. Alveolar bone associates intramembranous and endochondral bones. Mesenchymal stem cells (osteoprogenitor cells) initiate bone mineralization including a differentiation cascade. Alveolar bone includes pre-osteoblasts, osteoblasts, osteocytes, and bone lining cells, all these cells being derived from hematopoietic stem cells. The alveolar bone extracellular matrix (ECM) includes collagens, elastins, glycosaminoglycans and proteoglycans, small leucine-rich proteoglycans, small integrin-binding ligand N-linked glycoprotein (phosphorylated SIBLINGs) (DSPP [fragmented after cleavage into dentin sialoprotein, dentin glycoprotein, and dentin phosphoprotein], phosphorylated proteins such as bone sialoprotein, matrix extracellular phosphorylated protein (MEPE), and osteopontin], non-collagenous non-phosphorylated proteins (osteonectin), serum derived proteins (α2-HS-glycoprotein, and albumin), specific and non-specific alkaline phosphatase, metalloproteinases and tissue inhibitors of metalloproteinases (TIMPs -1 to -4) and enzymes that regulate components of the alveolar bone. Osteoclasts are stimulating osteoclastogenesis, and consequently bone remodeling. ECM molecules are involved in bone mineralization or acting as mineralization inhibitors. The major functions of the alveolar bone are the following
- Providing structural support to teeth (Sharpey’s fibers)
- Act as mechanosensor
- Supply vascular nutrition and innervation, releasing neuromediators to the periodontal ligament
- Communicate with cells on the bone surface and with marrow cells
- Regulate blood-calcium and phosphate metabolism. Interactions between integrins-dependent extracellular molecules and bone cells are essential for bone formation and resorption. Studies have addressed the importance of the lacunocanalicular system and the pericellular fluid for the adaptation of bone to mechanical forces.
Keywords
Bone Lining Cells; Osteoblasts; Osteocytes; Osteoclasts; Sharpey’s Fibers; Collagens; Proteoglycans; SLRPs; SIBLINGs; MMPs; TIMPs; mineralization