Trevor Ottofaro1, Suvleen K Singh1, Richard J Friedman1, Josef K Eichinger1*
1Department of Orthopaedics and Physical Medicine, Medical University of South Carolina, Charleston, United States
*Correspondence author: Josef K Eichinger, Professor of Orthopaedics, Department of Orthopaedics and Physical Medicine, Medical University of South Carolina, Charleston, United States; Email: [email protected]
Published Date: 07-04-2023
Copyright© 2023 by Eichinger JK, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Given that optimization of management of the subscapularis is essential to ensuring an optimal outcome after shoulder arthroplasty, this review will focus on the ideal method of Lesser Tuberosity Osteotomy (LTO) repair and the methods by which this is assessed. Specifically, we will review the existing literature to determine how suture configuration, number of sutures, type of sutures, and osteotomy size all influence the biomechanics of an LTO repair.
Methods: A systematic review was performed in which one reviewer searched PubMed to find studies analyzing biomechanical strength of lesser tuberosity osteotomy repairs after a total shoulder arthroplasty. The following keywords were used to retrieve articles: (biomechanical) and (Lesser Tuberosity Osteotomy) or (LTO) or (subscapularis repair) and (total shoulder).
Results: Nine studies met inclusion criteria. LTO was the strongest, most durable repair in most biomechanical studies. However, the biomechanical testing protocols and repair techniques widely varied throughout the literature. Dual row repair with sutures wrapped around the stem as well thin LTO fragments showed superior biomechanical outcomes. There has been minimal literature focusing on how the number, size and type of suture utilized in a repair affect biomechanical outcomes.
Discussion: While the LTO repair technique has been demonstrated in multiple studies to be a biomechanically superior method of subscapularis repair in the setting of TSA, there has not been a single study which has analyzed the effects of repair technique, osteotomy size, as well as suture number/type/size using a standardized biomechanical testing protocol.
Level of Evidence: Level I; Biomechanics
Keywords: Subscapularis; Lesser Tuberosity Osteotomy (LTO); Total Shoulder Arthroplasty (TSA); Biomechanics; Repair; Strength
Abbreviation
LTO: Lesser Tuberosity Osteotomy; TSA: Total Shoulder Arthroplasty; ST: Subscapular Tenotomy; MTS: Materials Testing Systems
Introduction
Total Shoulder Arthroplasty (TSA) is an increasingly common surgical procedure. Over the past 10 years, multiple studies have shown that the number of total shoulder arthroplasties increased by 89% [1]. A key portion of shoulder arthroplasty is release of subscapularis to allow for adequate exposure and in turn appropriate component positioning. There are multiple techniques described for subscapularis release since the advent of TSA. In 1974, Neer, et al., first described subscapularis mobilization via a Subscapular Tenotomy (ST) [2]. This involved a tenotomy 1 cm medial to its insertion on the Lesser Tuberosity (LT) with subsequent end to end repair. However, there was concern regarding subscapularis dysfunction. One of the first research studies addressing potential complications was Miller et al reporting abnormal results in 67.5% liftoff and 66% of belly press examinations [3]. Over the years, numerous articles have reported post-op dysfunction and complete rupture significantly worsens clinical outcomes. This prompted many surgeons to explore alternatives for subscapularis mobilization and repair. These alternatives included subscapular peel and LTO.
The Lesser Tuberosity Osteotomy (LTO) was first described by Gerber, et al., in 1999, which involved osteotomy of part of the lesser tuberosity with subscapularis attached and subsequent bone to bone repair [4]. Theorized benefits of this included no violation of the subscapularis tendon, increased strength of bone-bone healing, and the ability to monitor healing/integrity of repair via XRs. This review will focus on biomechanical assessment of LTO. Given that optimization of management of the subscapularis is essential to ensuring an optimal outcome after shoulder arthroplasty, this review will focus on the ideal method of LTO repair and the methods by which this is assessed. Specifically, we will review the existing literature to determine how suture configuration, number of sutures, type of sutures, and osteotomy size all influence the biomechanics of an LTO repair.
Materials and Methods
A systematic review was performed in which one reviewer searched PubMed to find studies analyzing biomechanical strength of lesser tuberosity osteotomy repairs after a total shoulder arthroplasty. The following keywords were used to retrieve articles: (Biomechanical) and (LTO) or (Subscapularis repair)) and (total shoulder). This yielded 114 articles. Inclusion criteria were studies that were written in English and analyze biomechanical outcomes of lesser tuberosity osteotomy subscapularis repair after a TSA and/or reverse TSA. This ultimately resulted in 9 articles which met our inclusion criteria.
Biomechanical Assessment
Methods of biomechanical testing used in research studying and comparing the LTO to other modes of subscapularis mobilization are largely similar. This is involving cadaveric shoulders dissected of all musculature with the exception of the subscapularis and potting them in epoxy. Subsequently, the subscapularis was attached to a Materials Testing Systems (MTS) Instron or similar device (Shore Western servohydralic load frame in Simovitch) to apply specific force at a specified rate and number of cycles. This method and the parameters for testing the subscapularis repair were largely based on supraspinatus muscle testing, as ideal parameters of testing of the subscapularis were not as well studied. Of note, the method by which the subscapularis was attached to the MTS did vary. Of the studies that specifically stated their method of attachment, a majority reported securing the tendon to the device via a cryo-jaw. Additionally, the position of the humerus during biomechanical studies also varied somewhat amongst studies, mainly with regards to abduction. The cadaveric humeri were most often tested in 0-45 degrees of abduction, neutral rotation, and 135-degree line of pull to match the physiologic direction of pull [5].
More specifically, two studies (Fishman, et al., and Ahmad, et al.,) used identical testing protocols [5,6]. This involved the shoulder specimen being preloaded to 5 N for 1 min and subsequently underwent increasing cyclic loads for 40 cycles at 0.25 Hz. Increments were then increased by 25 N until 250 N or failure. Heckman, et al., preloaded cadaveric specimens to 10 N and then subjected to cyclic loading of 180 N at a rate of 1 Hz of 500 cycles [7]. Specimens were then held at 10 N for 10 seconds then loaded to complete failure at a rate 1 mm/second. Four other studies (Giuseffi, et al., Ponce, et al., Schmidt, et al., Buraimoh, et al.,) used a very similar biomechanical method in which they cyclically loaded specimens to 100 N (Buramioh. et al., loaded to 75 ± 50 N) at a rate of 1 Hz for 3000 cycles [8-11]. In the case of 2 studies, those specimens that remained intact after cyclic loading were then subjected to maximum load to failure with a loading rate of 33 mm/second. Giuseffi, et al., performed maximal load to failure at loading rate of 2 mm/s [8]. In the case of Buraimoh, et al., after the initial 3000 cycles at 75 ± 50 N, specimens underwent incremental cyclical loading where they increased undulation point by 25 N every 300 cycles until catastrophic failure or up to a final load of 450 ± 50 N, which corresponded to a total of 7500 cycles [3]. Another two studies (Van Thiel, et al., and Virk, et al.,) used similar protocol involving preloading shoulder specimens to 10 N for 1 min [12,13]. They were cyclically loaded for 150 cycles from 10 to 100 N at 0.5 Hz. After cyclic testing, each specimen was pulled to failure at a rate of 1 mm/s.
Using the methods described above, multiple variables were measured to assess the biomechanical properties of the repair. A majority of studies available assessed cyclic displacement, maximum load of failure and mode of failure. Other variables assessed included initial displacement, total displacement, stiffness, gross rotational motion. Displacement of LTO or other subscapularis repairs was assessed in most studies. Multiple studies used a differential variable reluctance transducer to assess displacement. Additionally, one must consider how each of the studies defined failure of the subscapularis repair. While most studies defined failure based on catastrophic or gross failure (suture pull out, fracture of LTO fragment, etc.) others used specific measurements to define failure. For example, Krishnan et al and Heckman et al both defined failures as 100% displacement of the LTO fleck from the donor site [8,10]. Additionally, Heckman et al defined failure within the tenotomy group as 5 mm gapping in the tendon repair [8]. This variation in definition of failure may in some circumstances underestimate, and others overestimate, the biomechanical strength of a construct. Additionally, while gross or catastrophic failure of a repair would certainly correlate with clinical failure, it is difficult to assess whether more subtle definitions of failure would be clinically significant.
Despite the wide variation in methods of assessing displacement, maximum load to failure, and other biomechanical outcomes, multiple studies cite their rationale for their protocol as the study by Bull et al, which found the subscapularis experiences 135 N of force during resistance to 30 N ER load [2,7]. The number of cycles also varies amongst studies; however, Giuseffi, et al., performed 3000 cycles bases on an estimated post-operative PT regime (70 repetitions daily for 6 weeks) [8].
Results
Repair Technique
In reviewing the biomechanical studies assessing LTO repairs, there were multiple different methods of LTO repair utilized in the existing literature to date. With regards to suture configuration, there were three main repair techniques encountered:
- Compression suture
- Tension suture
- Dual Row or CornRow repair
A compression suture LTO repair relies on a suture which encircles the entire osteotomy to apply compression at the site. This was accomplished in a varied manner using different number/type/size of sutures, drill holes, and incorporation of the implant. Two studies simply used two parallel rows of holes on either side of the osteotomy to pass suture transosseously around the implant (Fig. 1) [7,13]. Krishnan, et al., used a similar technique with the addition of passing the suture through the subscapularis tendon (Fig. 2) [10]. In contrast, Fishman et al studied two different methods of compression sutures [5]. One involved 5 drill holes to pass suture laterally, around the stem and out the medial aspect of humerus, then through the tendon with addition of a titanium cable in the middle hole (Fig. 3) [5]. The other technique simply involved two sutures (Fig. 3) [5].
An alternative method for repairing an LTO is via a tension suture technique. This involves passing a suture through the humerus and out of the greater tuberosity. Gerber et al was one of the first to describe this technique in 2006.6 Gerber’s technique involved four 2mm holes drilled medial to the bicipital groove and out through the greater tuberosity. The LTO was performed and then the implant was placed. Subsequently, a suture was placed transosseously through one hole at the bone-tendon junction then through a bone tunnel adjacent to the starting drill hole and tied over a base plate at the greater tuberosity. Another suture is then placed in the remaining two holes. This allows the suture to grasp the tendon at the bone interface and travel over the lesser tuberosity, thus acting as hinge laterally and allowing subscapularis contraction to close down any gapping. Four studies were found to have used a tension LTO repair technique (Fig. 4) as described originally by Gerber (Buraimoh, et al., Van den Berghe, et al., Heckman, et al., and Van Thiel, et al.,) [1,11,12,14]. However, one study (Schmidt et al) tested a combination of both tension and compression techniques (Fig. 5) [15].
Lastly, a dual row or Corn-row repair technique is also described in the literature for repair of LTO (Fig. 6) [10]. This was popularized by Krishnan, et al., in 2009. Their original article describes a medial and lateral row of sutures used for repair. The lateral row consists of four sutures passed through the bone-tendon interface of the subscapularis and then transosseously through the osteotomy bed from medial to lateral. This row is similar to the compression technique described above. For the medial row, four sutures are passed transosseously from the anatomic neck through the cut surface of the humeral head. They are then passed through the capsulotendinous subscapularis in horizontal mattress fashion. The lateral row functions. Thus, overall, the lateral row sutures function to compress the fleck osteotomy containing the subscapularis tendon insertion, while the medial row restores the capsulotendinous attachment of the anatomic neck.
Sutures
While some studies have compared various repair techniques and specifically compared compression and tension repair techniques, few have directly compared the effect that number and type of suture used has on ultimate load to failure and cyclic displacement of LTO subscapularis repairs. Three studies (Giuseffi, et al., Krishnan, et al., Ponce, et al.,) used 4 #5 sutures [8,9,17]. Two studies (Ahmad, et al., Heckman, et al.,) used 4 number 2 sutures to repair LTO [5,7]. The remainder of biomechanical studies used varied number, type, and diameter of sutures to repair LTOs. Looking at the extremes, Heckman, et al., and Schmidt, et al., used the fewest suture for their LTO repair (2 #2 sutures) [7,10]. In contrast, Krishnan, et al., used the highest number of sutures (8 #5 sutures) [17]. Although a paucity of data exists on suture type and number on biomechanical outcomes, meta-analysis does show that techniques using 3-4 sutures had a 39% great load to failure when load to failure compared to using two sutures.18 Additionally, #5 suture had 29% greater mean load to failure compared to #2 suture [18].
Osteotomy Size
Only one study (Schmidt, et al.,) specifically analyzed LTO size and biomechanical outcomes [10]. Specifically, Schmidt et al used a CT scan to compare thick and thin osteotomies that were both repaired through compression and tension suture configurations. In this study, the ideal thick osteotomy was 100% of the tuberosity height and thin was 50% of the tuberosity height. They found that a thin LTO fragment (40-50% of height) had less initial displacement and a lower rate of failure at the osteotomy site compared to thick LTO fragments. Additionally, they found that the strongest overall repairs regardless of osteotomy size were those that combined tension and compression sutures. Thus, based on their analysis, the ideal repair thin LTO fragment with a combination of compression and tension sutures. However, it is worth noting that there was no significant difference in load to failure between the two groups. While prior studies have not directly, compared osteotomy size some have made note of their LTO fragment size. Ponce, et al., used a thin (4-5 mm) osteotomy fragment with 4 #5 FiberWire sutures [9]. In contrast, Gerber, et al., recommend a large osteotomy (5-10 mm) to avoid suture pulling through the osteotomy fragment [7]. However, their study offers no specific biomechanical analysis.
Clinical Outcomes
While biomechanical data offers some insight into strength and durability of varying LTO techniques, clinical outcomes are the ultimate determinate of a successful and functional repair of subscapularis after a shoulder arthroplasty. Additionally, radiographic imaging can be useful in determining the success of an LTO repair. Post-op imaging can show if the LTO has healed properly or if it is in the correct location as seen on the original pre-op X-ray. Fig. 7,8 show the pre-operative and post-operative X-rays of a successful LTO repair. Early data by Ponce, et al., demonstrated 93% of patients had intact subscapularis function at 15 months.15 5 patients were noted to have dysfunction and only 1 rupture. Furthermore, all 76 patients had radiographic union. However, Ponce’s study lacked a control group. Multiple other studies examining clinical outcomes of LTO subscapularis repair have compared this to alternative methods of repair, including tenotomy and peel. Two studies (Lapner, et al., and Levine, et al.,) performed RCT comparing LTO to SP and ST, respectively, reported no significant difference in clinical outcomes or muscle strength [17]. However, multiple other studies have found difference in outcomes and subscapularis strength between LTO and alternative methods of repair [4,16]. When comparing LTO to tenotomy, multiple retrospective studies have demonstrated improved functional outcome, but many of these represent low level evidence. Scalise, et al., demonstrated less ultrasound evidence of subscapularis attenuation in LTO repairs in comparison to tenotomy, which in turn correlated with greater Penn Shoulder Scores in the LTO group [16]. The most recent study examining clinical outcomes of LTO compared to alternative methods of subscapularis management is a systematic review and meta-analysis by Del Core, et al., in 2020 [20]. This study demonstrated that the LTO cohort had greater IR range of motion and strength, which did not reach significance, as well as significantly fewer positive belly press tests. Overall, LTO patients had the greatest percentage of normal results for the belly-press, lift-off and shirt-tuck tests. Additionally, in comparison to ST and SP cohorts, LTO repairs demonstrated significantly higher healing rates. Unfortunately, this meta-analysis was unable to compare patient reported outcomes amongst the three subscapularis repair methods, but did note excellent post-operative outcomes amongst all 3 groups.
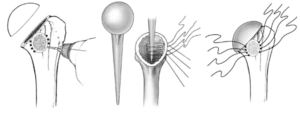
Figure 1: Compression suture passed transosseously around the implant using parallel rows of holes.
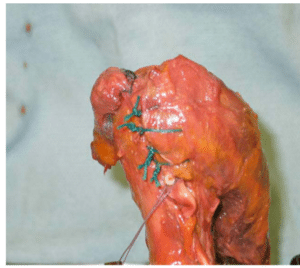
Figure 2: Single row technique passing #4 #5 ethibond sutures through tendon medial to bone fleck and then transosseously through osteotomy site and out lateral to bicipital groove.
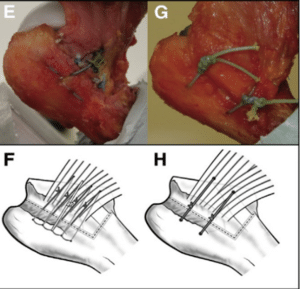
Figure 3: Two different methods of compression sutures.
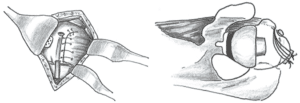
Figure 4: Tension suture technique.
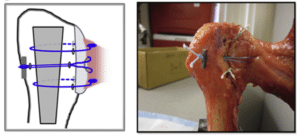
Figure 5: Tension and compression suture repair.
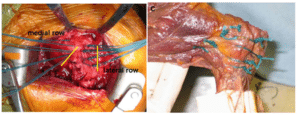
Figure 6: Dual row repair.

Figure 7: Pre-op X-ray of lesser tuberosity.
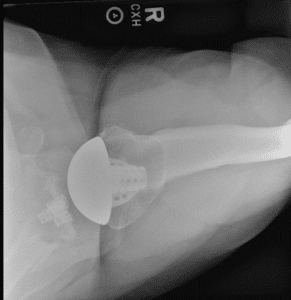
Figure 8: Post-op X-ray of LTO repair.
Discussion
LTO was the strongest, most durable repair in most biomechanical studies. However, the biomechanical testing protocols and repair techniques widely varied throughout the literature. There are numerous variables, as highlighted above, which may affect the biomechanics of an LTO subscapularis repair. First, the repair technique widely varies amongst studies. Heckman, et al., demonstrated that a dual row technique was significantly stronger and had less cyclic displacement than a backpack (aka tension band) repair [8]. Additionally, multiple studies demonstrated superior biomechanical outcomes with those LTO techniques that involved sutures around the humeral stem [5,7,10,15,17,18]. Another consideration is osteotomy size. Schmidt, et al., demonstrated thin LTO fragments had less displacement and lower rate of failure compared to thick fragments [10]. Finally, one most also consider the number, size and type of suture utilized in a repair. This is perhaps the most variable and least well studied factor within the existing body of literature. Schrock, et al., did report that those repairs with 3-4 sutures or #5 suture (as opposed to #2) did have greater load to failure [18].
In regards to clinical outcomes, there is not clear data demonstrating the superiority of LTO subscapularis repair, or any alternative method for that matter. Two RCTs demonstrated no difference in PROM or muscle strength amongst the various methods of subscapularis management after TSA [11,12]. However, other studies have demonstrated significantly improved IR strength as well as ultrasound subscapularis integrity after an LTO repair, which correlates with PROM, in comparison to alternative techniques [16-20]. Overall, studies examining clinical outcomes also tend to be limited due variability in data collection and outcome measures. For example, there is a wide variation amongst clinical studies as to what exam maneuvers are used to assess subscapularis integrity, including: IR ROM, IR strength, belly press, shirt tuck, and lift off. Additionally, even amongst studies using the same physical exam maneuvers, there is wide variation as to how the exam is performed.
Conclusion
In conclusion, the LTO repair technique has been demonstrated in multiple studies to be a biomechanically superior method of subscapularis repair in the setting of TSA, there has not been a single study which has analyzed the effects of repair technique, osteotomy size, as well as suture number/type/size using a standardized biomechanical testing protocol. Particularly, there is a paucity of literature that exists on the number, size, and type of suture to be used for a biomechanically ideal LTO repair. Given the variability and, in some instances, absence of data regarding the ideal method of LTO repair, we propose that future research should investigate how suture, osteotomy size, and method of repair affect biomechanical outcomes of LTO repairs. Additionally, the literature is also lacking in a truly standardized method to assess clinical outcomes of subscapularis repair methods. Future research could focus on larger size studies using standardized physical exam maneuvers and patient report outcome measures to elucidate if one method of repair is clinically superior to others.
Conflict of Interest
The authors have no conflict of interest to declare.
References
- Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am. 2011;93(24):2249-54.
- Neer CS. 2nd Replacement arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 1974;56(1):1-13.
- Levine WN, Munoz J, Hsu S, Byram IR, Bigliani LU, Ahmad CS, et al. Subscapularis tenotomy versus lesser tuberosity osteotomy during total shoulder arthroplasty for primary osteoarthritis: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2019;28(3):407-14.
- Gerber C, Pennington SD, Yian EH, Pfirrmann CA, Werner CM, Zumstein MA. Lesser tuberosity osteotomy for total shoulder arthroplasty. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1)170-7.
- Ahmad CS, Wing D, Gardner TR, Levine WN, Bigliani LU. Biomechanical evaluation of subscapularis repair used during shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16(3 Suppl):S59-64.
- Fishman MP, Budge MD, Moravek JE, Jr Mayer M, Kurdziel MD, Baker KC, et al. Biomechanical testing of small versus large lesser tuberosity osteotomies Bull AM, Reilly P, Wallace AL, Amis AA, Emery RJ. A novel technique to measure active tendon forces: application to the subscapularis tendon. Knee Surg Sports Traumatol Arthrosc. 2005;13(2):145-50.
- Heckman DS, Hoover SA, Weinhold PS, Spang JT, Creighton RA. Repair of lesser tuberosity osteotomy for shoulder arthroplasty: biomechanical evaluation of the backpack and dual Row techniques. J Shoulder Elbow Surg. 2011;20(3):491-6.
- Giuseffi SA, Wongtriratanachai P, Omae H, Cil A, Zobitz ME, An KN, et al. Biomechanical comparison of lesser tuberosity osteotomy versus subscapularis tenotomy in total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(8):1087-95.
- Ponce BA, Ahluwalia RS, Mazzocca AD, Gobezie RG, Warner JJ, Millett PJ. Biomechanical and clinical evaluation of a novel lesser tuberosity repair technique in total shoulder arthroplasty. J Bone Joint Surg Am. 2005;87(Suppl 2):1-8.
- Schmidt CC, Jarrett CD, Brown BT, DeGravelle M, Jr, Sawardeker P, Weir DM, et al. Effect of lesser tuberosity osteotomy size and repair construct during total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(1):117-27.
- Buraimoh MA, Okoroha KR, Oravec DJ, Peltz CD, Yeni YN, Muh SJ. A biomechanical comparison of subscapularis repair techniques in total shoulder arthroplasty: lesser tuberosity osteotomy versus subscapularis peel. JSES Open Access. 2018;2(1):8-12.
- Van Thiel GS, Wang VM, Wang FC, Nho SJ, Piasecki DP, Bach BR Jr, et al. Biomechanical similarities among subscapularis repairs after shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19(5):657-63.
- Virk MS, Aiyash SS, Frank RM, Mellano CS, Shewman EF, Wang VM, et al. Biomechanical comparison of subscapularis peel and lesser tuberosity osteotomy for double-row subscapularis repair technique in a cadaveric arthroplasty model. J Orthop Surg Res. 2019;14(1):391.
- Van den Berghe GR, Nguyen B, Patil S, D’Lima DD, Mahar A, Pedowitz R, et al. A biomechanical evaluation of three surgical techniques for subscapularis repair. J Shoulder Elbow Surg. 2008;17(1):156-61.
- Fishman MP, Budge MD, Moravek JE, Jr Mayer M, Kurdziel MD, Baker KC, et al. Biomechanical testing of small versus large lesser tuberosity osteotomies: effect on gap formation and ultimate failure load. J Shoulder Elbow Surg. 2014;23(4):470-6.
- Krishnan SG, Stewart DG, Reineck JR, Lin KC, Buzzell JE, Burkhead WZ. Subscapularis repair after shoulder arthroplasty: biomechanical and clinical validation of a novel technique. J Shoulder Elbow Surg. 2009;18(2):184-92.
- Lapner PL, Sabri E, Rakhra K, Bell K, Athwal GS. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94(24):2239-46.
- Miller SL, Hazrati Y, Klepps S, Chiang A, Flatow EL. Loss of subscapularis function after total shoulder replacement: A seldom recognized problem. J Shoulder Elbow Surg. 2003;12(1):29-34.
- Schrock JB, Kraeutler MJ, Crellin CT, McCarty EC, Bravman JT. How should I fixate the subscapularis in total shoulder arthroplasty? A systematic review of pertinent subscapularis repair biomechanics. Shoulder Elbow. 2017;9(3):153-9.
- Del Core MA, Cutler HS, Ahn J, Khazzam M. Systematic review and network meta-analysis of subscapularis management techniques in anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30(7):1714-24.
Article Type
Review Article
Publication History
Received Date: 07-03-2023
Accepted Date: 31-03-2023
Published Date: 07-04-2023
Copyright© 2023 by Eichinger JK, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Eichinger JK, et al. Systematic Review of Lesser Tuberosity Osteotomy Techniques, Outcomes and Biomechanical Testing Parameters: A Critical Appraisal. J Ortho Sci Res. 2023;4(1):1-10.
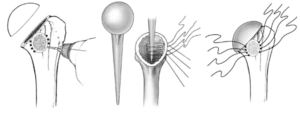
Figure 1: Compression suture passed transosseously around the implant using parallel rows of holes.
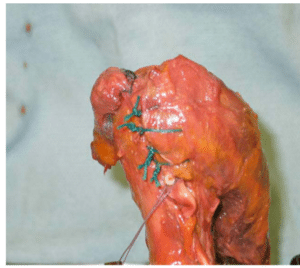
Figure 2: Single row technique passing #4 #5 ethibond sutures through tendon medial to bone fleck and then transosseously through osteotomy site and out lateral to bicipital groove.
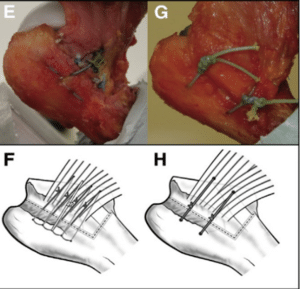
Figure 3: Two different methods of compression sutures.
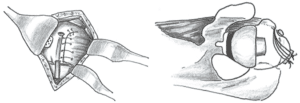
Figure 4: Tension suture technique.
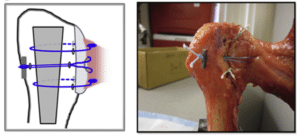
Figure 5: Tension and compression suture repair.
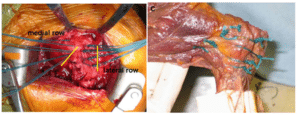
Figure 6: Dual row repair.

Figure 7: Pre-op X-ray of lesser tuberosity.
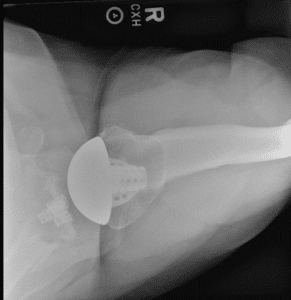
Figure 8: Post-op X-ray of LTO repair.