Cortical Mandibular Bone Blocks Grafts and Piezoelectric Surgery in Complex Anterior Maxillary Alveolar Defects: A Case Report and Literature Review
Thomas G Wiedemann1*
1Clinical Associate Professor, Department of Oral and Maxillofacial Surgery, New York University College of Dentistry, New York, United States
*Correspondence author: Thomas G Wiedemann, MD, PhD, DDS, Clinical Associate Professor, Department of Oral and Maxillofacial Surgery, New York University College of Dentistry, New York, United States; Email: tgw1@nyu.edu
Citation: Wiedemann TG. Cortical Mandibular Bone Blocks Grafts and Piezoelectric Surgery in Complex Anterior Maxillary Alveolar Defects: A Case Report and Literature Review. Jour Clin Med Res. 2023;4(2):1-6.
Copyright© 2023 by Wiedemann TG. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 25 Jul, 2023 | Accepted 10 Aug, 2023 | Published 18 Aug, 2023 |
Abstract
The aim of this study is to assess the indication and efficacy of alveolar ridge reconstructions for complex horizontal and vertical augmentation procedures in the maxillary anterior area with Cortical Mandibular Bone Block Grafts (CMBBG).
Localized alveolar three-dimensional bone defects are among the most challenging problems in surgical implant dentistry. Treatment protocols, such as short implants or small diameter implants are not always offering the desired clinical and esthetic results.
The autogenous augmentation procedure can serve as an option, which allows a more biological reconstruction of the vertical and horizontal dimension of a complex bone defect in order to obtain sound replicas of natural teeth.
The clinical case of a cortical autogenous block graft in an anterior complex maxillary defect is presented along with a literature review. The presented case and the selected articles demonstrate that cortical ramus bone block grafts show relatively low graft resorption, low donor site morbidity and high implant success rates.
Keywords: Autologous Bone Grafts; Bone Defect; Ramus Graft; Cortical Block Graft; Bone Augmentation; Piezoelectric Surgery
Introduction
Different bone reconstructive or regenerative techniques have been proposed in the past: distraction osteogenesis, maxillary sinus floor elevation, onlay grafts with intraoral and extraoral autogenous bone blocks, guided bone regeneration with resorbable or non-resorbable membranes in association or not with tenting screws; and protected bone regeneration with non-customized or customized titanium meshes [1-6].
The autogenous block graft is still considered as the method of choice for three-dimensional and complex bone augmentation procedures in severely resorbed maxillary anterior alveolar segments. Bone augmentation can be performed using either bone blocks, particulate bone or a combination of both. The donor site can be either intraoral or extraoral. The mandibular ramus is the most preferable donor site.
The aim of this case study is to report and present the efficacy of alveolar ridge reconstructions for complex horizontal and vertical augmentation procedures in the maxillary anterior area with a cortical mandibular bone block graft from a retromolar donor site.
Material and Methods
An electronic search using PubMed and Google Scholar has been performed by utilizing keywords such as: “mandibular block graft” and “anterior maxilla”, “ramus graft”, “onlay intraoral block graft”, “autogenous augmentation”. References were selected based on systematic reviews, meta-analysis and randomized clinical trials written in the English language and published in highly respected international journals selected relevant articles were evaluated for data extraction [7]. Moreover, articles for comparison and discussion were further hand searched and selected without date restriction. The obtained information was evaluated for its significance to support autogenous bone grafts as gold standard in complex alveolar bone defects. 14 articles and one reference book have been selected.
Results
A 41-year-old male patient has been referred to the Department of Oral and Maxillofacial Surgery at NYU Dentistry for implant evaluation of an edentulous site of the left central incisor. The tooth has been extracted about 18 months ago. The patient’s medical history was non-remarkable. Intraorally, the edentulous site of the left maxillary central incisor presented with a severe horizontal post-extraction bone loss and a partial loss of the buccal plate. CBCT evaluation revealed 3 mm alveolar bone width (Fig. 1). Due to the complexity and amount of bone loss, a cortical autogenous block graft was indicated. After the preparation of the donor site, the graft was harvested from the ascending ramus by using an ultrasonic device. The graft was then adjusted and anchored in the residual maxillary bone using small diameter titanium micro screws (Fig. 2). The spaces between the cortical bone graft and the residual bone were filled with particulated harvested bone collected with a safe scraper and covered with a resorbable collagen membrane. A Vascularized Palatal Connective Tissue Flap (VIP-CT) and horizontal mattress sutures were used for safe wound coverage and adaptation (Fig. 3). No post-operative complications were noted. The implant has been inserted 4 months following the augmentation without any intra- or postoperative complications or further grafting procedures.
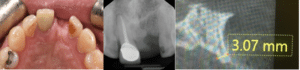
Figure 1: Preoperative clinical and radiographical evaluation showing a complex horizontal bone defect. CBCT evaluation revealed 3mm residual alveolar bone width.

Figure 2: Intraoperative view with cortical block graft anchored in the residual maxillary bone using small diameter titanium microscrews.
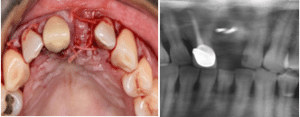
Figure 3: Vascularized palatal connective tissue flap and horizontal mattress sutures used for safe wound coverage and soft tissue adaptation.
The most relevant clinical results of our literature review revealed:
- Cortical ramus bone block grafts show a relatively low graft resorption (0.23 – 1.86 mm)
- Implant success rates in grafted sites are ranging between 93.1 – 100% during a 6 – 33 months of follow-up periods (Table 1), showing similar success rates compared to implant placements in pristine bone
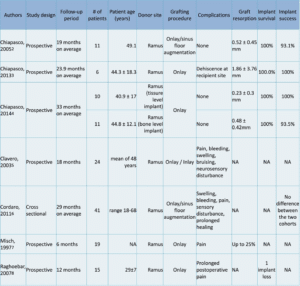
Table 1: Evaluation of the literature review.
Discussion
Bone grafts from intraoral donor sites offer several benefits like surgical accessibility, proximity of donor and recipient sites, less discomfort for the patient and less morbidity as compared with extraoral locations. The choice of the intraoral donor site is usually based on the amount, geometry, and type of bone required for alveolar reconstruction. Additionally, the incidence of intra- and postoperative complications should be considered [8].
The main advantage of a cortical mandibular ramus graft technique is that cortical block grafts are harvested from the external oblique ridge with a piezotome, making the procedure very safe and with a low risk of complications. Moreover, the amount of the bone block to be harvested can be reduced considerably, making the procedure much less invasive.
Cortical bone blocks are initially used to restore the contours of the alveolar ridge and the remaining gaps are then filled with autogenous bone chips. The resulting accelerated vascularization in the gap between the graft and the ridge and the volume stability of the avascular cortical bone plate reduces bone resorption to less than 10%, so the alveolar ridge contour can be restored with a predictable outcome [9]. The short-and long-term results after augmentation with the aid of the bone shell technique demonstrated low complication rates and excellent volume stability, even 10 years after surgery [10]. The ramus should be considered the site of choice when block grafts are needed for horizontal or vertical augmentation for maxilaary anterior bone defects [11].
In addition, autologous onlay-grafts from the mandibular ramus offer sufficient bone volume to reconstruct the atrophic jaw segment without long-lasting harvesting morbidities. This site is an excellent treatment alternative with high patient acceptance when reconstruction is necessary before implant insertion. Besides a successful reconstruction of the alveolar crest with correct selection of the donor site, patient acceptance of the procedure is high, while the morbidity of the procedure is minimal showing no persistent nerve damage, which is considered the main disadvantage of autologous bone grafts in the past. The contribution of the use of piezoelectric surgery, grafting templates, and guided implant insertion to the reported result cannot not be addressed in this article, but with the described technique, predictable outcomes and lacking lasting morbidities can be achieved independently from surgical level and status of the provider. Based on the authors experience the piezoelectric technique is a safe method to prevent nerve damage and can be recommended in autologous intraoral bone harvesting. Studies have demonstrated that the harvesting technique plays an essential role in the process of graft consolidation [12]. This is usually attributed to the impact of the harvesting technique on the viability and activity of the transplanted cells. It has been shown that cell viability and the release of molecules affecting bone formation were higher in samples harvested by a bone scraper, like in the presented case, when compared with samples prepared by bone drilling [13].
The author attributed the low graft resorption to the short healing period of 4 months, which has proven to be sufficient for the revascularization of the graft and the secure insertion of dental implants as suggested in the past by various authors [14,15]. Therefore, it is suggested to limit the healing period after autologous bone grafting to a maximum of 4-5 months. This leads to earlier dental restorations compared to augmentations using bone substitutes, where the healing periods are often recommended up to 12 months [16].
The most relevant innovations in bone grafting during the past few years , such as computer- aided design/computer- aided manufacturing technologies have allowed customizing titanium meshes or bone/bone substitute blocks (e.g., computer- guided bone harvesting procedures, three- dimensional- printed bone models or allograft plates, three- dimensional- printed allogenic/xenogeneic/alloplastic bone blocks, etc.), are further reducing treatment time and restoring geometrically complex anatomic defects with accuracy and precision.
Future trends in bone defect augmentation may rely on new concepts in regenerative medicine and tissue engineering using stem cells on three- dimensional- printed scaffolds. However, their use is currently limited to research environments because of costs and legislation, but it is crucial that they provide additional benefits over current standard therapies (ie, guided bone regeneration, bone shell technique with autogenous bone) [17-24].
Conclusion
When considering the low harvesting morbidity and invasiveness, autogenous cortical ramus grafts still remain the “gold standard” in complex and advanced alveolar ridge reconstructions with resorption of the buccal plate prior to implant placement.
We recommend a two – stage surgical protocol which includes connective tissue augmentation and implant placement approximately four months after the grafting procedure.
Conflict of Interest
The author has no conflict of interest to declare.
References
- Nkenke E, Neukam FW. Autogenous bone harvesting and grafting in advanced jaw resorption: morbidity, resorption and implant survival. Eur J Oral Implantol. 2014; 7 (Suppl2):S203-17.
- Chiapasco M, Casentini P, Zaniboni M, Corsi E. Evaluation of peri-implant bone resorption around Straumann bone level implants placed in areas reconstructed with autogenous vertical onlay bone grafts. Clin Oral Implants Res. 2012;23:1012-21.
- Chiapasco M, Autelitano L, Rabbiosi D, Zaniboni M. The role of pericranium grafts in the reduction of postoperative dehiscences andbone resorption after reconstruction of severely deficient edentulous ridges with autogenous onlay bone grafts. Clin Oral Implants Res. 2013;24:679-87.
4.Chiapasco M, Casentini P, Zaniboni M. Implants in reconstructed bone: A comparative study on the outcome of Straumann Tissue Level and Bone Level Implants placed in vertically deficient alveolar ridges treated by means of autogenous onlay bone grafts. Clin Implant Dent Relat Res. 2014.
- Clavero J, Lundgren S. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res. 2003;5:154-160.
- Cordaro L, Torsello F, Miuccio MT, di Torresanto VM, Eliopoulos D. Mandibular bone harvesting for alveolar reconstruction and implant placement: subjective and objective cross-sectional evaluation of donor and recipient site up to 4 years. Clin Oral Implants Res. 2011;22:1320-6.
- Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997;12:767-76.
- Raghoebar GM, Meijndert L, Kalk WW, Vissink A. Morbidity of mandibular bone harvesting: a comparative study. Int J Oral Maxillofac Implants. 2007;22:359-65.
- Clementini M, Morlupi A, Agrestini C, Ottria L. Success rate of dental implants inserted in autologouus bone graft regenerated areas: a systematic review. Oral and Implantology. 2011:3-4.
- Khoury F, Hanser T. Mandibular bone block harvesting from the retromolar region: a 10-year prospective clinical study. Int J OralMaxillofac Implants. 2015;30(3):688-97.
- Urban I, Montero E, Sanz-Sánchez I. Minimal invasiveness in vertical ridge augmentation. Periodontol 2000. 2023:1-19.
- Chiapasco M, Consolo U, Bianchi A, Ronchi P. Alveolar distraction osteogenesis for the correction of vertically deficient edentu-lous ridges: a multicenter prospective study on humans. Int J Oral Maxillofac Implants. 2004;19(3):399-407.
- Chin M, Toth BA. Distraction osteogenesis in maxillofacial surgery using internal devices: review of five cases. J Oral Maxillofac Surg. 1996;54(1):45-54.
- Roccuzzo M, Ramieri G, Bunino M, Berrone S. Autogenous bone graft alone or associated with titanium mesh for vertical alveolar ridge augmentation: a controlled clinical trial. Clin Oral Implants Res. 2007;18(3):286-94.
- Her S, Kang T, Fien MJ. Titanium mesh as an alternative to a membrane for ridge augmentation. J Oral Maxillofac Surg. 2012;70(4):803- 10.
- Miyamoto I, Funaki K, Yamauchi K, Kodama T, Takahashi T. Alveolar ridge reconstruction with titanium mesh and autogenous particulate bone graft: computed tomography- based evaluations of augmented bone quality and quantity. Clin Implant Dent Relat Res. 2012;14(2):304-11.
- Briguglio F, Falcomata D, Marconcini S, Fiorillo L, Briguglio R, Farronato D. The use of titanium mesh in guided bone regenera-tion: a systematic review. Int J Dent. 2019;2019:9065423.
- Sumida T, Otawa N, Kamata YU. Custom- made titanium de-vices as membranes for bone augmentation in implant treatment: clinical application and the comparison with conventional titanium mesh. J Craniomaxillofac Surg. 2015;43(10):2183- 8.
- Sagheb K, Schiegnitz E, Moergel M, Walter C, Al- Nawas B, Wagner W. Clinical outcome of alveolar ridge augmentation with individualized CAD-CAM- produced titanium mesh. Int J Implant Dent. 2017;3(1):36.
- Sakkas, A., Wilde, F., Heufelder, M: . Autogenous bone grafts in oral implantology-is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int J Implant Dent. 2017;3:23.
- Heberer S, Rühe B, Krekeler L, Schink T, Nelson JJ, Nelson K. A prospective randomized split-mouth study comparing iliac onlay grafts in atrophied edentulous patients: covered with periosteum or a bioresorbable membrane. Clin Oral Implants Res. 2009;20:319-26.
- Semper W, Kraft S, Mehrhof J, Nelson K. Impact of abutment rotation and angulation on marginal fit: theoretical considerations. Int J Oral Maxillofac Implants. 2010;25:752-8.
- Miron RJ, Gruber R, Hedbom E. Impact of bone harvesting techniques on cell viability and the release of growth factors of autografts. Clin Implant Dent Relat Res. 2013;15:481-9.
- Buser D. 30 years of guided bone regeneration. 3rd Edition, Quintessence Publishing. 1994.
This work is licensed under a Creative Commons Attribution 2.0 International License.


