A Huge Retroperitoneal Large B-Cell Lymphoma Presenting As Chronic Small Bowel Obstruction: A Case Report
Ningi AB1*, Aliyu S2, Adewunmi OL2, Zarami AB2
1- Department of Surgery, Abubakar Tafawa –Balewa University, Bauchi state, Nigeria
2- Department of Surgery, University of Maiduguri Teaching Hospital, Borno state, Nigeria
*Corresponding Author: Ningi Adamu Bala, Department of Surgery, Abubakar Tafawa –Balewa
University, Bauchi state, Nigeria; Tel: +2348066160193; Email: abningi@yaoo.com; ningibala41@gmail.com
Citation: Ningi AB, Aliyu S, Adewunmi OL, Zarami AB. A Huge Retroperitoneal Large B-Cell Lymphoma Presenting As Chronic Small Bowel Obstruction: A Case Report. J Clin Med Res. 2020;1(1):1-12..
Copyright© 2020 by Ningi AB, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 04 Apr, 2020 | Accepted 13 Apr, 2020 | Published 20 Apr, 2020 |
Abstract
Retroperitoneal tumours are an aggregate of multiple types of neoplastic lesions with a preponderance of tumours of mesenchymal origin. Other histological types such as Lymphoma, are reported to be commoner now. Retroperitoneal tumours are generally rare and clinical diagnosis is often difficult due its cryptic location. It is often diagnosed incidentally following abdominal radiological studies or following complications. The most common complication being an extrinsic compression, particularly, on the retroperitoneal structures; such as the ureters, duodenum or the major abdominal vessels. It may also present as a vague abdominal pain or chronic bowel obstruction like our index patient. Abdominal CT Scan is the most sensitive tool of diagnosis and complete surgical excision often, an enbloc excision with involved adjoining organs offers the best chance of cure. Adjuvant chemotherapy, radiotherapy or chemo-radiation improve disease free interval and overall survival. The mainstay of retroperitoneal lymphoma is however a cytotoxic chemotherapy or more recently Rituximab combination therapy.
We present a case of a huge retroperitoneal large B-cell Lymphoma presenting as chronic small bowel obstruction.
Keywords
Retroperitoneal Tumour; Chronic Intestinal Obstruction; Large B-cell Lymphoma
Introduction
Retroperitoneal Tumours (RPT) are rare and the most common variety is the retroperitoneal lymphoma. Retroperitoneal sarcomas are the most common differential. They are a rare and heterogeneous group of tumours and the Sarcomas arise from the supporting extra-skeletal tissues in the retroperitoneum [1]. In the United State of America (USA), it is estimated that 10-20% of all diagnosed soft tissue sarcomas are from the retroperitoneum, at a prevalence of 0.3-0.4 cases/100,000 population [2]. Clinical diagnosis of retroperitoneal tumours is often delayed as most of these tumours are asymptomatic until they become very large [3]. The average size at diagnosis was reported to be 15-18 cm [4-6]. The gold standard for diagnosis is contrast enhanced Abdomino-pelvic CT Scan. It gives a good soft tissue delineation, can provide an idea of tumour variety and a safe image guided biopsy can be taken [7]. Although CT scan of the chest is sufficient to rule out metastasis, MRI may be preferable in patients with known allergy to intravenous contrast and also where an assessment of spinal foramina, nerves, and posterior muscles involvement is required [8]. The retroperitoneal location and the contiguity with adjacent vital structures such as, the aorta, inferior vena cava, duodenum, head of the pancreas, ureters and gonadal vessels make surgical excision and adjuvant radiotherapy hazardous, because these structures have poor tolerance to radiation energy [9,10]. Postoperative tumour recurrence is said to be high [11]. Several studies from developed countries have shown that radical surgical resection and the use of advanced radio-therapeutic approach have reduced the recurrence rates [12].
The Trans-Atlantic RPS Working Group (TARPSWG), a transatlantic collaboration of multiple specialized sarcoma centres, published its consensus guidelines for the management of recurrent RPS. It advocated a multimodal treatment and a careful review of postoperative histopathologic reports [13]. The oncologic outcome has been observed to be worse with each surgical resection and the risk of developing life threatening morbidities increases with each repeat surgery [14]. An abysmal prognosis is a feature for retroperitoneal tumours. A 36-58% 5-year Overall Survival (OS) and a high tendency for late recurrences have been reported [15]. The histological grade of RPT is an important prognostic factor. About two-thirds of RPT are of intermediate or high grade and one-third are low grade [16]. Intermediate or high-grade tumours have a tendency for distant metastasis, most often, involving the lung and liver. Low-grade tumours have the risk of local recurrence rather than distant metastases [17,18].
Tumours arising from the lymphatic structures give rise to lymphoma and the retroperitoneal position is said to be the most common location [19,20]. The retroperitoneal lymphoma has been noted to have greater tendency for forming composite soft tissue masses than lymphomas located in other parts of the body [21].
There is a dearth of reports from Africa highlighting the presentation of retroperitoneal tumour with chronic bowel obstruction and even rarer is a report of retroperitoneal lymphoma. We present our experience of managing such a presentation and the peculiar postoperative histopathological diagnosis.
Case Report
A 46-year-old farmer presented at the emergency room of University of Maiduguri Teaching Hospital in Borno state, Nigeria with clinical features of chronic small bowel obstruction. He narrated an 11-year history of recurrent constipation relieved by laxative ingestion and a repeated episode of vague abdominal pain. There was history of significant weight loss over 6 months prior to presentation and also a history of episodic drenching night sweats. Symptoms were not given importance by the general practitioner in his area of domicile as the patient complained during the summer in the arid region of North-Eastern Nigeria. There was no previous history of abdominal surgery or reducible groin swellings. No Mycobacterium Tuberculosis was detected on Gene-X-pert analysis of his sputum. Patient presented at the tertiary health facility on self-referral. Physical examination revealed a chronically ill patient with clinical signs of acute intestinal obstruction. There was however a distinctly palpable, hard, irregular solid mass occupying the right upper and lower abdominal quadrants. The bowel loops and the liver were displaced medially.
Patient was resuscitated with Hartman’s solution and preoperative haematological and biochemical panels were done. A plain erect and supine radiographs indicated a small bowel obstruction. A complimentary abdominal USS demonstrated the huge intra-abdominal mass and right hydro-ureter and hydronephrosis. An abdominal CT scan or an Intravenous Urogram were not done as patient couldn’t afford the cost and was not a beneficiary of the National Health Insurance. Patient was prepared for and had an open exploratory laparotomy.
Surgery
A long midline incision was used and on peritoneal breach there was no presence of straw-coloured or haemorrhagic effluent. The mass was noticed to be retroperitoneal with displacement of the liver, small and large bowels medially. There were no peritoneal tubercles or carcinomatosis peritonei and the liver appeared free of nodules. The right colon was mobilised medially by dividing the relatively avascular lateral parietal peritoneum along the line of Toldt. The hepatico-colic and the gastro-colic ligaments were clamped and divided. The major abdominal vessels, the second part of the duodenum and the pancreatic head, the right kidney and the renal vessels were identified and found to be free, off the well capsulated mass. The duodenum, pancreatic head and the Inferior venacava were gently dissected off the mass. The renal, gonadal and iliac vessels were also isolated and dissected free from the mass. There was no infiltration of the psoas muscle, the right ureter or the femoral nerve. Adequate retraction was applied to the anterior abdominal wall and the mass excised under direct vision. Haemostasis was secured and the tumour bed lavaged with warm distilled water. No drain was placed at the tumour bed and the abdomen was closed by massive closure. The mass was complex, consisting of solid and cystic components and weighed 16 kg. About 10 lts of turbid exudative effluent was drained. No hair, teeth or bone was seen within its cavity. Histopathologic reported indicated a low grade, large B-cell Lymphoma. Patient was referred to the clinical haematology unit for adjuvant chemotherapy. He declined adjuvant radiotherapy due to financial constraints (Fig.1-8).

Figure 1: Showing the grossly distended abdomen with obvious right upper quadrant fullness.

Figure 2: Showing the mobilised retroperitoneal mass and the displaced liver.

Figure 3: Showing the mobilised mass and the displaced bowel loops.

Figure 4: Showing the tumour bed.

Figure 5: Showing the completely excised mass.

Figure 6: Showing the areas of haemorrhage and necrosis within the cavity of the mass.
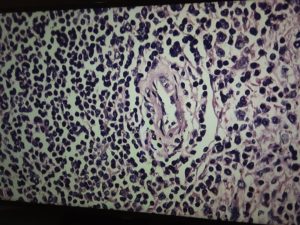
Figure 7: Histopathology slide of B-cell lymphoma.
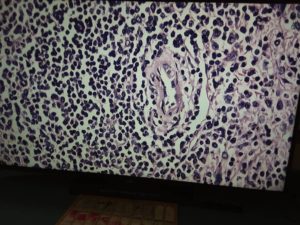
Figure 8: Showing the histopathology slide of large B-cell lymphoma.
Discussion
Retroperitoneal masses have been a source of diagnostic conundrum to the surgeon. The intervening peritoneal contents often are source of the presenting symptoms from extrinsic compression and they also mask clinical signs on palpation. Diagnosis is often delayed and the mass lesions often assume a significant size before they are recognised. The early parts of the 19th century came with improved diagnostic imaging tools, such as PET scan and scintigraphy, Computed Tomographic (CT) scanning and magnetic resonance imaging [22-26].
Obtaining tissue biopsy has been an albatross until these imaging technologies allowed image guided percutaneous fine-needle biopsies. Diagnostic laparotomy, hitherto, the only diagnostic method was limited to situations where the minimally invasive diagnostic methods failed [27,28]. Improvements in diagnostic technology allowed for more sophisticated biopsy procedures to be routinely performed under local anaesthesia as a day case procedure [27,29].
Haematological malignancies are rare compared to malignant lesions of epithelial origin. There is no reliable data from Nigeria, as there are only 4 functional cancer registries. Reports from the USA indicated that lymphomas generally constituted approximately 4% of all cancers in the 1970s and it declined to a 2% annual increase from the 1990s [30]. The report also indicated a higher incidence among Caucasians. The incidence of Non Hodking Lymphoma (NHL) in white women was approximately 11.5/100,000 person years. A total of 60,000 cases diagnosed over a 17-year period were studied and the incidence in black women was placed at 40% lower. Low-grade B-cell lymphomas belongs to the NHL group and consist of mainly small lymphocytic lymphoma, follicular lymphoma, marginal-zone B-cell lymphoma, and lympho-plasmacytic lymphoma [31].
Several reports have described Lymphoma as the most frequent malignant tumour in the retroperitoneum [32,33]. Although many studies indicated a female preponderance, there are other reports with a male predominance [34-37]. The low grade B-cell lymphoma is known to affect people in the middle age group, has a peak age of 55-60 years [38]. Our patient presented at 46 years of age. Perhaps, due to extrinsic mechanical bowel obstruction. Cancers generally are said to be seen at a decade earlier in the black African patient compared to a Caucasian [39]. Low-grade B-cell lymphomas, especially follicular lymphoma, tend to have an intractable course with a median survival as long as 7 to 10 years. It often advances in to a higher histological grade, commonly, the diffuse large B-cell lymphoma [40].
Presentation with advanced disease is common, as in our patient. A report from USA indicated that 75-90% of Caucasian patients are diagnosed with retroperitoneal lymphoma at advanced Ann Arbor Clinical Stage (CS) III-IV, frequently with bone marrow involvement and Follicular lymphomas are responsible for advanced low-grade B-cell lymphomas [41].
The mainstay of treatment of NHL is non-operative multi-modal therapy and regardless of location, NHL is highly responsive to cytotoxic chemotherapy, except those with high grade biological profile. Early stage, slowly growing retroperitoneal NHL can be treated successfully with radiotherapy, especially, the nodular or follicular type. External beam radiotherapy, however may result in debilitating retroperitoneal fibrosis, radiation enteritis or pyelonephritis [42]. The first line chemotherapy for diffuse B-cell lymphoma is Rituximab in combination with Cyclophosphamide, Doxorubicin, Vincristine and Prednisone (R-CHOP) [43]. Patients with high risk for CNS metastasis are given prophylactic intrathecal methotrexate or cytarabine. These include patients with bone marrow, testicular, nasal/paranasal, orbital, skeletal, or peripheral blood dissemination [44]. Adjuvant radiation therapy is given, but, its relevance is being questioned as no statistically significant difference was observed between those given cytotoxic monotherapy and those with adjuvant radiation therapy [45].
Surgical resection is deployed in the treatment of retroperitoneal lymphoma, especially, a diffuse B-cell lymphoma with a huge mass lesion with extrinsic compression of adjoining organs. This may involve an En bloc resections of the involved organs. A microscopically free margin (R0) resection is the goal of surgical resection. The median survival period of 500 patients treated for RPT was found to have improved by over 7 years (85 months) with complete R0 resection [46].
A staggering 40-70% has been reported to be the histologic transformation rate of follicular lymphoma and the average interval between diagnosis and histologic transformation is said to be 4 to 5 and a half year. The median survival after histologic transformation is very poor, estimated to be less than 1 to 2 years [47,48]. The overall survival is therefore worse than that of moderate and high grade diseases [49]. The 5-year survival is 60-80%, 10-year survival placed at 50-60% [49]. Poor overall survival result also from higher stage at presentation and the finding of an unresectable disease or positive surgical margins [38].
Conclusion
Retroperitoneal lymphoma is a rare disease and presentation is often as advanced disease. Vague abdominal pain may be the only symptom unless there is an extrinsic compression or infiltration of contiguous structures. The goal of treatment should be a complete remission or curative resection. An R0 resection improves both disease free survival and overall survival. A high index of suspicion should be maintained in the management of any patient with recurrent vague abdominal pain and progressive abdominal distension.
References
- Fletcher CD, Unni KK, Mertens F, editors. Pathology and genetics of tumours of soft tissue and bone. IARC; 2002.
- Mettlin C, Priore R, Rao U, Gamble D, Lane W, Murphy GP. Results of the national soft‐tissue sarcoma registry. J Surg Oncol. 1982;19(4):224-7.
- Park JO, Qin LX, Prete FP, Antonescu C, Brennan MF, Singer S. Predicting outcome by growth rate of locally recurrent retroperitoneal liposarcoma:“the one centimeter per month rule”. Annals of surgery. 2009;250(6):977-82.
- Stojadinovic A, Yeh A, Brennan MF. Completely resected recurrent soft tissue sarcoma: primary anatomic site governs outcomes. J Am Col Surg. 2002;194(4):436-47.
- Gyorki DE, Brennan MF. Management of recurrent retroperitoneal sarcoma. J Surg Oncol. 2014;109(1):53-9.
- Hassan I, Park S, Donohue J, Nagorney D, Kay P, Nasciemento A, et al. Operative management of primary retroperitoneal sarcomas: a reappraisal of an institutional experience, Ann. Surg. 2004;239(2):244-50.
- Messiou C, Morosi C. Imaging in retroperitoneal soft tissue sarcoma. J Surg Oncol. 2018;117:25-32.
- Sinziana D, Alessandro G. The diagnosis and management of retroperitoneal sarcoma. Oncology (Williston Park, N.Y.) 2018:32(9). Last accessed on 02 April 2020 https://www.researchgate.net/publication/327868937
- Chun-qiu C, Lu Y, Cheng-hong P, Yong C, Ya-fen L, Ren Z, et al. Prognostic factors of retroperitoneal soft tissue sarcomas: analysis of 132 cases, Chin. Med J. 2007;120(12):1047-50.
- Gronchi A, De Paoli A, Dani C, Merlo DF, Quagliuolo V, Grignani G, et al. Preoperative chemo-radiation therapy for localised retroperitoneal sarcoma: A phase I–II study from the Italian Sarcoma Group. Eur J Cancer 2014;50(4):784-92.
- Garcia-Ortega DY, Villa-Zepeda O, Martinez-Said H, Cuellar-Hübbe M, Luna-Ortiz K. Oncology outcomes in retroperitoneal sarcomas: prognostic factors in a retrospective cohort study. Int J Surg. 20161;32:45-9.
- Mullinax JE, Zager JS, Gonzalez RJ. Current diagnosis and management of retroperitoneal sarcoma. Cancer Control. 2011;18(3):177-87.
- Trans-Atlantic RPS Working Group. Management of recurrent retroperitoneal sarcoma (RPS) in the adult: a consensus approach from the Trans-Atlantic RPS Working Group. Ann Surg Oncol. 2016;23(11):3531-40.
- MacNeill AJ, Miceli R, Strauss DC, Bonvalot S, Hohenberger P, Van Coevorden F, et al. Post‐relapse outcomes after primary extended resection of retroperitoneal sarcoma: a report from the Trans‐Atlantic RPS Working Group. Cancer. 2017;123(11):1971-8.
- Porter GA, Baxter NN, Pisters PW. Retroperitoneal sarcoma: a population‐based analysis of epidemiology, surgery, and radiotherapy. Cancer. 2006;106(7):1610-6.
- Ardoino I, Miceli R, Berselli M, Mariani L, Biganzoli E, Fiore M, et al. Histology‐specific nomogram for primary retroperitoneal soft tissue sarcoma. Cancer. 2010;116(10):2429-36.
- Gronchi A, Collini P, Miceli R, Valeri B, Renne SL, Dagrada G, et al. Myogenic differentiation and histologic grading are major prognostic determinants in retroperitoneal liposarcoma. Am J Surg Pathol. 2015;39(3):383-93.
- Huang HY, Brennan MF, Singer S, Antonescu CR. Distant metastasis in retroperitoneal dedifferentiated liposarcoma is rare and rapidly fatal: a clinicopathological study with emphasis on the low-grade myxofibrosarcoma-like pattern as an early sign of dedifferentiation. Mod Pathol. 2005;18(7):976-84.
- Elsayes KM, Staveteig PT, Narra VR, Chen ZM, Moustafa YL, Brown J. Retroperitoneal masses: magnetic resonance imaging findings with pathologic correlation. Curr Probl Diagn Radiol. 2007;36(3):97-106.
- Guo PD, Xian JF, Man FY, Liu ZH, Yan F, Zhao J, et al. Magnetic resonance imaging features of extraocular muscle lymphoma in five cases. Chin Med J. 2016;129(19):2384.
- Bakir B, Yilmaz F, Turkay R, Ozel S, Bilgiç B, Velioglu A, et al. Role of diffusion-weighted MR imaging in the differentiation of benign retroperitoneal fibrosis from malignant neoplasm: Preliminary study. Radiology 2014;272:438-45.
- Fox K, Silfen D, Alavi A. Applications of gallium-67 scintigraphy in the management of patients with malignant lymphoma. J Nucl Med. 1991;32:2299-305.
- Cohen-Haguenauer O, Brice P, Gaci M, Le AP, Cheval E, Bris C, et al. Gallium-67 scintigraphy in malignant lymphoma. Presse Med. 1993;22(11):521-5.
- Strijk SP. Lymphography and abdominal computed tomography in the staging of non-Hodgkin lymphoma. Acta Radiol. 1987;28:263-9.
- Hoane BR, Shields AF, Porter BA, Borrow JW. Comparison of initial lymphoma staging using computed tomography (CT) and magnetic resonance (MR) imaging. Am J Hematol. 1994;47(2):100-5.
- Skillings JR, Bramwell V, Nicholson RL, Prato FS, Wells G. A prospective study of magnetic resonance imaging in lymphoma staging. Cancer. 1991;67(7):1838-43.
- Erwin BC, Brynes RK, Chan WC, Keller JW, Phillips VM, Gedgaudas‐McClees RK, et al. Percutaneous needle biopsy in the diagnosis and classification of lymphoma. Cancer. 1986;57(5):1074-8.
- Castellino RA, Hoppe RT, Blank N, Young SW, Neumann C, Rosenberg SA, et al. Computed tomography, lymphography, and staging laparotomy: correlations in initial staging of Hodgkin disease. AJR Am J Roentgenol. 1984;143(1):37-41.
- Suzuky T, Schibuya H, Yoshimatsu S. Ultrasonically guided staging splenic tissue core biopsy in patients with non-Hodgkin lymphoma. Cancer. 1987;60:879-82.
- Müller AM, Ihorst G, Mertelsmann R, Engelhardt M. Epidemiology of non-Hodgkin’s lymphoma (NHL): trends, geographic distribution, and etiology. Ann Hematol. 2005;84(1):1-2.
- Krol AD, Le Cessie S, Snijder S, Kluin-Nelemans JC, Kluin PM, Noordijk EM. Primary extranodal non-Hodgkin’s lymphoma (NHL): the impact of alternative definitions tested in the Comprehensive Cancer Centre West population-based NHL registry. Ann Oncol. 2003;14(1):131-9.
- Armstrong JR, Cohn Jr I. Primary malignant retroperitoneal tumors. Am J Surg. 1965;110(6):937-43.
- Braasch JW, Mon AB. Primary retroperitoneal tumors. Surg Clin North Am. 1967;47(3):663-78.
- Waldron Jr JA, Newcomer LN, Katz ME, Cadman E. Sclerosing variants of follicular center cell lymphomas presenting in the retroperitoneum. Cancer. 1983;52(4):712-20.
- Ampil FL. Malignant lymphoma presenting in the retroperitoneum. Oncology. 1989;46(3):198-200.
- Melicow MM. Primary tumors of the retroperitoneum; a clinicopathologic analysis of 162 cases; review of the literature and tables of classification. J Int Coll Surg.1953;19(4):401-9.
- Pack GT, Tabah EJ. Primary retroperitoneal tumors: a study of 110 cases. Int Abstr Surg. 1954; 99:313-41.
- Chiappa A, Zbar AP, Bertani E, Biffi R, Luca F, Crotti C, et al. Primary and recurrent retroperitoneal soft tissue sarcoma: prognostic factors affecting survival. J Surg Oncol. 2006;93(6):456-63.
- Aliyu S, Babayo UD, Tahir MB, Zarami AB, Ibrahim AG, Madziga AG. Colorectal Cancer in Maiduguri North-Eastern Nigeria. Palgo J Med.Medical Sci. 20175;191-3.
- Izumo T, Maseki N, Mori S, Tsuchiya E. Practical Utility of the Revised European‐American Classification of Lymphoid Neoplasms for Japanese Non‐Hodgkin’s Lymphomas. Jpn J Cancer. 2000;91(3):351-60.
- Portlock CS. Management of the low-grade non-Hodgkin’s lymphomas. Semin Oncol. 1990;17:51-59.
- Ballo MT, Zagars GK, Pollock RE, Benjamin RS, Feig BW, Cormier JN, et al. Retroperitoneal soft tissue sarcoma: an analysis of radiation and surgical treatment. Int J Radiat Oncol Biol Phys. 2007;67(1):158-63.
- Adult Non-Hodgkin Lymphoma Treatment. 2015; Last accessed on 02 April, 2020 http://www.cancer.gov/cancertopics
- 44. Abramson JS, Hellmann M, Barnes JA, Hammerman P, Toomey C, Takvorian T, et al. Intravenous methotrexate as central nervous system (CNS) prophylaxis is associated with a low risk of CNS recurrence in high‐risk patients with diffuse large B‐cell lymphoma. Cancer. 2010;116(18):4283-90. 45.
- Horning SJ, Weller E, Kim K, Earle JD, O’Connell MJ, Habermann TM, et al. Chemotherapy with or without radiotherapy in limited-stage diffuse aggressive non-Hodgkin’s lymphoma: Eastern Cooperative Oncology Group study 1484. J Clin Oncol. 2004;22(15):3032-8.
- Lewis JJ, Leung D, Woodruff JM, Brennan MF. Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg. 1998;228(3):355.
- 47. Acker B, Hoppe RT, Colby TV, Cox RS, Kaplan HS, Rosenberg SA. Histologic conversion in the non-Hodgkin’s lymphomas. J Clin Oncol. 1983;1(1):11-6.
- Krikorian JG, Portlock CS, Cooney DP, Rosenberg SA. Spontaneous regression of non‐Hodgkin’s lymphoma: A report of nine cases. Cancer.1980;46(9):2093-9.
- Rosenberg SA. Karnofsky memorial lecture. The low-grade non-Hodgkin’s lymphomas: challenges and opportunities. J Clin Oncol. 1985;3(3):299-310.
This work is licensed under Attribution-NonCommercial-NoDerivs 2.0 Generic (CC BY-NC-ND 2.0) International License. With this license readers are free to share, copy and redistribute the material in any medium or format as long as the original source is properly cited.

