A Rare Case of Evans Syndrome Associated with Underlying Dermatomyositis Without Generalized Subcutaneous Edema: A Case Report
Brian Shaw1, Mohammad Karaman1, Rameez Rao2, Ryan Shaw3, Steve J Carlan4*
1Department of Internal Medicine, USA
2Department of Pulmonology, USA
3University of South Florida, Biomedical Sciences Department, Tampa, Florida, USA
4Division of Academic Affairs and Research, USA
*Correspondence author: Steve J Carlan, Division of Academic Affairs and Research, Orlando, Florida, USA; Email: stevecarlan@gmail.com
Citation: Jamali M, et al. Exploring the Intricacies of Encephalitis in Mosquito-Borne Diseases through Vector-Host-Pathogen Interactions: A Critical Review. Jour Clin Med Res. 2023;4(3):1-10.
Copyright© 2023 by Carlan SJ, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 05 Dec, 2023 | Accepted 24 Dec, 2023 | Published 31 Dec, 2023 |
Abstract
Background: Primary Evans Syndrome is a typically idiopathic systemic illness associated with a number of autoimmune conditions and lymphomas and characterized by Coombs-positive warm-agglutinin Autoimmune Hemolytic Anemia (AIHA) and immune thrombocytopenia. The disease can be severe and prolonged with multiple recurring disease flares. Its association with dermatomyositis remains exceedingly rare and all reported cases have been accompanied by generalized subcutaneous edema.
Case Report: We report a case of a 24-year-old male with a decade-long medical history of Evans Syndrome who presented to the emergency room with a one-week history of shortness of breath and fatigue. An extensive workup revealed severe anemia, thrombocytopenia and a left hemothorax. Active intervention included video-assisted thoracoscopy with decortication, blood products and autoimmune investigation. He was ultimately diagnosed with dermatomyositis after an electromyograph showed findings consistent with demyelinating peripheral polyneuropathy of motor nerves.
Conclusion: Evans syndrome associated with dermatomyositis is extremely rare and this is to our knowledge the first reported case of Evans syndrome associated with dermatomyositis without generalized subcutaneous edema.
Keywords: Evans Syndrome; Autoimmune Disease; Dermatomyositis; Hemolytic Anemia
Introduction
Evans syndrome is characterized by the simultaneous or sequential occurrence of Coombs-positive warm-agglutinin Autoimmune Hemolytic Anemia (AIHA) and Immune Thrombocytopenia (ITP) without an underlying origin and may present with or without immune neutropenia [1]. Thrombocytopenia, anemia and neutropenia may be severe and prolonged resulting in a progressive decline of health despite treatment. Primary Evans syndrome is typically idiopathic, but Evans syndrome has been associated with a number of autoimmune conditions and lymphomas [2]. Despite Evans syndrome’s association with autoimmune conditions, its association with dermatomyositis remains exceedingly rare with only 6 cases in the literature. [3-8] Dermatomyositis is an inflammatory disease that primarily affects the proximal muscle groups in a symmetric fashion with a number of extramuscular manifestations [9]. Based on the 6 cases described, each time dermatomyositis is associated with Evans syndrome, it is also accompanied by generalized subcutaneous edema [3-8]. Evans syndrome is not commonly associated in the literature as a predisposing factor for other autoimmune conditions. Here we present an atypical case of Evans syndrome associated with dermatomyositis in which a 24-year-old with an established history of Evans syndrome developed underlying dermatomyositis without generalized subcutaneous edema leading to repeated flares of his Evans syndrome.
Case Presentation
This is a case of a 24-year-old male with a long medical history of Evans Syndrome who presented to the emergency room with a one-week history of shortness of breath and fatigue. The patient described himself as physically active and regularly played flag football with his friends. He denied fevers, chills, sick contacts, or recent travel. The patient suffered chronically from Evans syndrome since early adolescence and had been receiving blood transfusions nearly weekly for years due to increasingly frequent flares. The patient noted skin changes on both hands evolving over the past few years that he believed to be warts and bilateral calf pain for the past few months. On presentation to the ED his vitals were stable. Initial laboratory values were significant for very low hemoglobin (4.1 g/dL) ([12.6-16.7g/dL]) and platelet count (11 x 103µL) ([139-361 x 103µL]). Imaging was significant for a complex collection of fluid overlying the entire left hemithorax (Fig. 1). On physical exam, the patient had decreased breath sounds over the left chest with dullness to percussion. The patient had a dull purple rash around his eyes as well as facial flushing. Additionally, the patient had suspicious bilateral dorsal Proximal Interphalangeal (PIP) and Metacarpophalangeal (MCP) joint plaques (Fig. 2).
Case Presentation
This is a case of a 24-year-old male with a long medical history of Evans Syndrome who presented to the emergency room with a one-week history of shortness of breath and fatigue. The patient described himself as physically active and regularly played flag football with his friends. He denied fevers, chills, sick contacts, or recent travel. The patient suffered chronically from Evans syndrome since early adolescence and had been receiving blood transfusions nearly weekly for years due to increasingly frequent flares. The patient noted skin changes on both hands evolving over the past few years that he believed to be warts and bilateral calf pain for the past few months. On presentation to the ED his vitals were stable. Initial laboratory values were significant for very low hemoglobin (4.1 g/dL) ([12.6-16.7g/dL]) and platelet count (11 x 103µL) ([139-361 x 103µL]). Imaging was significant for a complex collection of fluid overlying the entire left hemithorax (Fig. 1). On physical exam, the patient had decreased breath sounds over the left chest with dullness to percussion. The patient had a dull purple rash around his eyes as well as facial flushing. Additionally, the patient had suspicious bilateral dorsal Proximal Interphalangeal (PIP) and Metacarpophalangeal (MCP) joint plaques (Fig. 2).
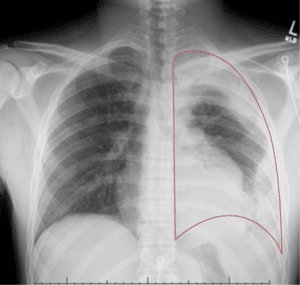
Figure 1: Complex collection of fluid overlying the entire left hemithorax. The red lines indicate the approximate lung borders, opacity within this space compared to the right side represents fluid overlying the lung. There is a complete loss of the costophrenic angle and evidence of fluid tracking both laterally and medially up to the superior portion of the lung.

Figure 2: Flat-topped, hyperkeratotic, scaly plaques on the PIP and MCP (black arrow) joints pathognomic for Gottron papules of dermatomyositis.
Lab Analysis | Value | Reference |
Hemoglobin | 4.1g/dL | 12.6-16.7g/dL |
Platelet Count | 11×103µL | 139-361×103µL |
Haptoglobin | <30mg/dL | 44-215mg/dL |
Lactate Dehydrogenase | 803U/L | 140-271U/L |
Direct Coombs (Igg) | Positive | Negative |
Cold Agglutinin | Negative | Negative |
Table 1: Laboratory results on admission.
Lab analysis | Value | Reference |
Anti-Nuclear Antigen (ANA) | 1:160 with a speckled pattern | Negative |
SS-A/Ro | Positive | Negative |
Anti-smooth muscle (IgG) | Positive | Negative |
Aldolase | 8.8U/L | <7.7U/L |
Table 2: Serum antibody results.
Discussion
There has been interest in recent years in classifying Evans syndrome as primary or secondary, the latter being associated with SLE, scleroderma, thyroid disease, other autoimmune conditions and certain lymphoproliferative disorders such as chronic lymphocytic leukemia [2]. It should be noted that primary Evans syndrome is a diagnosis of exclusion and a full autoimmune workup should be undertaken before making the diagnosis. Autoimmune conditions developing in the setting of Evans syndrome are not well documented in the literature. In our patient’s recalcitrant Evans syndrome, flares may be related to untreated dermatomyositis. This case highlights the importance of close follow-up and high clinical suspicion for new autoimmune conditions that may develop many years after the initial diagnosis of Evans syndrome with either new symptoms or flares of familiar symptoms. Despite Evans syndrome’s association with autoimmune conditions, its association with dermatomyositis is exceedingly rare with only 6 cases described in the literature to this point [3-8]. Of these, all were associated with generalized subcutaneous edema from dermatomyositis. Generalized subcutaneous edema was absent in our patient.
Dermatomyositis is characterized by one major criterion, either a characteristic skin finding or skin biopsy and at least four minor criteria including proximal muscle weakness, elevated muscle enzymes, positive myositis-specific antibodies, evidence of systemic inflammation and spontaneous muscle pains, among others, criteria our patient fulfilled [9]. Development of dermatomyositis is not benign and it is imperative that patients with a new diagnosis of dermatomyositis are screened for underlying malignancies especially in the first five years of diagnosis [9]. This highlights the importance of early diagnosis of secondary or underlying conditions in Evans syndrome as these can carry their own independent risks for greater disease burden related to late screening.
Management of Evans syndrome and dermatomyositis are similar with corticosteroids being first-line treatment and second-line treatments being steroid-sparing immunosuppressive drugs. IVIG is often added to corticosteroids in Evans syndrome depending on the extent of ITP [1,9]. Second-line therapy in Evans usually includes immunosuppressants such as rituximab, sirolimus, tavalisse and mercaptopurine. [1] As our patient did not respond to systemic corticosteroids alone, we started IVIG for a short period followed by oral cyclosporine with corticosteroids. For second-line treatment in dermatomyositis, azathioprine and methotrexate are frequently used and mycophenolate is preferred if there is pulmonary involvement [9]. Last line therapy for Evans syndrome includes splenectomy which our patient ultimately underwent.
Conclusion
There are four main conclusions to draw from this case. Firstly, Evans syndrome should prompt full autoimmune workup as it is a diagnosis of exclusion. Secondly, close follow-up of Evans syndrome over time is important as it may predispose patients to develop other autoimmune conditions such as dermatomyositis many years after the initial diagnosis of Evans syndrome. This is particularly true in patients with recalcitrant or frequently flaring Evans syndrome. Thirdly, surveillance and early diagnosis of secondary diagnoses are key as these conditions may carry their own sets of screening guidelines and concerns such as malignancy screening in dermatomyositis. These patients may benefit from repeated autoimmune workups as symptoms evolve. Lastly, Evans syndrome associated with dermatomyositis is extremely rare and this is to our knowledge the first reported case of Evans syndrome associated with dermatomyositis without generalized subcutaneous edema. Despite the rarity of the association, patients with dermatomyositis and anemia with or without subcutaneous edema should be evaluated for hemolysis and a new diagnosis of Evans syndrome should prompt thorough autoimmune workup and malignancy surveillance to rule out secondary associations.
Ethics Approval
The project did not meet the definition of human subject research under the purview of the IRB according to federal regulations and therefore was exempt.
Author Contributions
All listed authors have made a significant scientific contribution to the research in the manuscript approved its claims and agreed to be an author. Everyone made a significant scientific contribution. This is confirmation of the final authorship for this manuscript. No one else contributed to the manuscript. No one else qualifies for authorship.
Conflict of Interest
The authors have no conflict of interest to declare.
References
- Audia S, Grienay N, Mounier M, Michel M, Bonnotte B. Evans’ syndrome: from diagnosis to treatment. J Clin Medicine. 2020;9(12):3851.
- Shaikh H, Prerna M. Evans syndrome. StatPearls Publishing (2023).
- Hay EM, Makris M, Winfield J, Winfield DA. Evans’ syndrome associated with dermatomyositis. Annals Rheumatic Dis. 1990;49(10):793.
- Chang DK, Yoo DH, Kim TH, Jun JB, Lee IH, Bae SC, et al. Induction of remission with intravenous immunoglobulin and cyclophosphamide in steroid-resistant Evans’ syndrome associated with dermatomyositis. Clin Rheumatol. 2001;20:63-6.
- Jung KD, Kim PS, Park HY, Kim CR, Byun JY, Lee DY, et al. Dermatomyositis associated with generalized subcutaneous edema and Evans syndrome. J Am Acad Dermatol. 2012;66(1):144-7.
- Loja-Oropeza D, Zavala-Flores E, Vilca-Vasquez M. Dermatomiositis y síndrome de Evans asociado a infección por HTLV-1. Revista Peruana de Medicina Experimental y Salud Pública. 2016;33:162-7.
- Flores-Terry MA, Garcia-Arpa M, Anino-Fernandez J, Minguez-Sanchez MD. Edematous dermatomyositis with probable evans syndrome. Actas Dermo-sifiliograficas. 2017;108(7):673-5.
- Dal Lago L, Vandergheynst F, Awada A, Pepersack T. Rare features of dermatomyositis in a patient with ovarian cancer. Euro J Case Reports in Internal Medicine. 2020;7(12).
- Qudsiya Z, Waseem M. Dermatomyositis. StatPearls Publishing. 2023.
This work is licensed under a Creative Commons Attribution 2.0 International License.


