Garritano C1*, Godoy F2, Fonseca J2, Cruz LM2, Oliveira M2
1Department of General Surgery of the Federal University of the State of Rio de Janeiro, Brazil
2Resident Physician of General Surgery at Gaffrée and Guinle University Hospital, Federal University of the State of Rio de Janeiro, Brazil
*Corresponding Author: Garritano C, Department of General Surgery of the Federal University of the State of Rio de Janeiro, Brazil; Email: [email protected]
Published On: 24-03-2022
Copyright© 2022 by Garritano C, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Tuberculosis is among the top 5 causes of death from infectious disease caused by Mycobacterium tuberculosis, it most frequently affects the lungs, although it can compromise the digestive tract, genitourinary, peritoneum, pleura, bones, lymph nodes and meninges, composing the group of extrapulmonary tuberculosis. Peritoneal involvement is the most common form of abdominal type representing 0.1 to 0.7% of all tuberculosis cases. With nonspecific symptoms, without of laboratory findings that would guide the search for Mycobacteria and imaging tests that overlap common in other pathologies, the diagnosis is difficult. In Abdominal Computed Tomography, ascites, smooth peritoneal thickening, densification of the mesentery root, lymphadenomegaly with central necrosis or calcification are observed. Laparoscopy with the biopsy and collection of ascitic fluid is used as a method for diagnosis.
The mortality of abdominal tuberculosis can reach 15% and perforation of intestinal loops, malnutrition, anemia, hypoalbuminemia are the main complications. We present the case of a patient presenting recurrent umbilical hernia, whose diagnosis of peritoneal tuberculosis was made during surgery.
Keywords
Extra pulmonary Tuberculosis; Peritoneal Tuberculosis; Ascites
Introduction
Tuberculosis is among the top 5 causes of death from infectious diseases and the first among infectious diseases in HIV-infected patients [1,2].
Adults are the most affected by the disease and in 2020 men accounted for 56% of all cases, women for 33% and children for 11% [2].
There are several risk factors attributed to the onset of the disease, such as malnutrition, HIV infection, poverty, alcohol use, smoking and diabetes [2-4].
Caused by Mycobacterium tuberculosis, it affects the lungs more frequently, although it can also affect the abdomen, involving the digestive and genitourinary tract, abdominal aorta, peritoneum and abdominal lymph nodes, as well as the pleura, bones, lymph nodes and meninges, which are the extra pulmonary tuberculosis group [3-7].
Peritoneal involvement represents 0.1 to 0.7% of all types of tuberculosis, with the peritoneum being the 6th most-affected site [8].
We present the case of a young adult male patient with recurrent umbilical hernia, whose diagnosis of peritoneal tuberculosis was made during surgery.
Case Report
A 21-year-old male patient who, in May 2021, sought the General Surgery outpatient clinic, referring that for 3 years he had a painless bulging in the inguinal region, left scrotal bag and umbilical region. Ultrasonography showed intra-abdominal fat exteriorization during the Valsalva maneuver with an echographic aspect compatible with a scrotal inguinal hernia.
After laboratory and imaging tests that were normal, in June 2021 he underwent left inguinoscrotal hernioplasty, with polypropylene mesh placement and umbilical herniorrhaphy, which because of its small size, did not require a mesh. The patient progressed satisfactorily, being discharged from the hospital in a good clinical condition the day after surgery.
About 3 weeks after the surgical procedure, the patient returned with abdominal discomfort, nausea and loss of appetite. He denied respiratory symptoms, fever, or diarrhea. During the physical examination, he was lucid, oriented, afebrile and eupneic in room air; cardiac and pulmonary auscultation without alterations; distended abdomen with a voluminous umbilical hernia, painful to palpation with an orifice approximately 4 cm wide. Laboratory tests and chest X-rays were performed, which showed no alterations.
The patient was reoperated on and after the small trans-umbilical incision there was a slightly cloudy ascitic liquid of citrine aspect, more than 1500 ml of which was aspirated (Fig. 1).

Figure 1: Ascitic fluid collected during the surgery.
An enlargement of the surgical incision width was made to perform the inventory of the abdominal cavity and swollen, hyperemic intestinal loops with multiple whitish granulomatous lesions were identified (Fig. 2).

Figure 2: Aspect of jejunal loop.
They were also present in the peritoneum and appendix, that was congested and with an enlarged base (Fig. 3).

Figure 3: Aspect of appendix.
Several biopsies of peritoneal lesions, appendectomy and ascitic fluid collection were performed. The aspect of the changes in the abdominal cavity led us to think about the possibility of peritoneal tuberculosis.
In the postoperative period, the patient underwent a PPD test, HIV serology, syphilis, cytomegalovirus, hepatitis B and C, bacilloscopic exam and expert gene for tuberculosis.
All serologies and bacilloscopic exam were negative, as well as PPD. Ascitic fluid examination showed the presence of frequent lymphocytes, very rare reactive mesothelial cells, rare histiocytes, some red blood cells and lymphocytic effusion.
The histopathological result of the biopsy material showed granulomatous chronic peritonitis with giant cells, ecstatic blood vessels and granulomas sometimes with central necrosis. Granulomatous appendicitis, presence of giant cells; reactional hyperplasia of lymphoid tissue and the lumen of the organ filled with fibrino-leukocytic material. The findings suggest tuberculosis.
The patient was referred for follow-up and treatment at the Pulmonology division, immediately initiating the treatment recommended by the Brazilian Ministry of Health. At the same time, the disease began to be traced to family members, neighbors and people with constant contact with the patient to assess the existence of other contaminated individuals.
Discussion
The relationship between pulmonary disease and extra pulmonary tuberculosis was not understood until Laennec made an association between both in 1804. The term tuberculosis was introduced in 1839 and the first case of “tubercular peritonitis” occurred in a New York Hospital in 1843 [8-10].
Peritoneal tuberculosis is the most common form of abdominal tuberculosis that affects the peritoneal cavity, mesenteric and omentum, occurring in 11 to 12% of patients with extrapulmonary tuberculosis [4,5].
Peritoneal involvement represents 0.1 to 0.7% of all types of tuberculosis, with the peritoneum being the 6th most affected site, with the possibility of a simultaneous pulmonary disease involvement in 3.5% of the cases [8].
In the last decade, there has been an increase in the incidence of extrapulmonary tuberculosis globally and of the more than 6 million new cases of tuberculosis recognized by the WHO in 2017, 16% were extrapulmonary. Incidence rates ranged from 8% in the Western Pacific region to 24% in the Eastern Mediterranean [7,11,12].
It is noteworthy that in these references we found records of pleural, meningeal, lymphatic and skeletal extrapulmonary tuberculosis, but there is no mention of peritoneal involvement, which seems to be in the “other types” group.
According to the 2021 World Health Organization Global Report, the SARS-CoV-2 pandemic in 2020 was responsible for the highest number of deaths and the lowest number of cases diagnosed, treated, or under preventive treatment of tuberculosis compared to 2019. Due to the lockdown, tuberculosis treatment services were disrupted and human and financial resources were reallocated to the COVID-19 response, limiting the availability of essential services [1].
There are several theories to explain the onset of peritoneal tuberculosis, which may be the reactivation of latent foci implanted in the peritoneum during hematogenic dissemination, secondary to the rupture of mesenteric lymph nodes who were compromised by hematogenic dissemination of a distant primary focus, gastrointestinal dissemination, tubal involvement, direct and lymphatic extension [4-6,8].
There also seems to be a great association of peritoneal tuberculosis with other clinical pathologies such as: chronic liver disease, more precisely cirrhosis, chronic renal failure in continuous peritoneal dialysis, HIV peritoneal carcinomatosis, ovarian carcinoma and elevated levels of marked CA125 [13-17].
The major obstacle in diagnosis comes from nonspecific symptomatology because it is an insidious disease, without laboratory findings that would guide the search for Mycobacteria, the positivity of the test and by imaging that overlaps with those found in other pathologies [4-6,8].
The most affected age group is between 35 and 45 years old 8,10 and the most commonly reported symptoms are fever (60 to 75%), abdominal pain (65%) and weight loss (36 to 60%) which can be confused with other diseases and that in about 70% of cases may delay the diagnosis [4-10]. On physical examination, ascites (73%), pain on abdominal palpation (65 to 93%), hepatomegaly (28 to 52 %) and splenomegaly (14 to 21%) are observed [5.6,8,11,12].
In Abdominal Computed Tomography, the main findings are ascites (70% to 90% of cases); smooth peritoneal thickening with expressive enhancement after intravenous injection of the contrast medium; densification of the adipose planes of the mesentery root (70% of cases); lymphadenomegaly with areas of central necrosis or calcification [4].
According to macroscopic findings, peritoneal tuberculosis is classified into 3 types: dry (peritoneal and mesenteric thickening, caseous nodules, lymphadenomegaly and fibrous adhesions, found in approximately 3% of patients); wet (free or loculated ascites, associated or not with a smooth and diffuse peritoneal thickening); and fibrotic (sharp thickening of the epiploon, adhesion between intestinal loops, with or without loculated ascites simulating peritoneal carcinomatosis) [4,10].
Thus, laparoscopy with the biopsy of the lesions in the peritoneum and collection of ascitic fluid began to be used as an important method for diagnosis [8,10].
In the treatment of all forms of pulmonary and extrapulmonary tuberculosis, with the exception of meningoencephalitis, 4 drugs are recommended, namely: Rifampicin, Isoniazid, Pirazinamide and Ethabutol, known as the RIPE regimen [11-19]. The WHO recommends the simultaneous use of intravenous antibiotics and there is also a reference for the use of corticosteroids in the first months of treatment in the abdominal forms of the disease in order to avoid intestinal obstruction [3,11]. Even with satisfactory results with the RIPE regimen, many patients do not complete treatment or don’t do it properly. The rate of treatment abandonment in Brazil in 2017 reached 10.3% [2].
The mortality of abdominal tuberculosis can reach 15%, with perforation of intestinal loops, malnutrition, anemia, hypoalbuminaemia and postoperative complications referred to as the main factors [20].
We present the case of a 21-year-old patient, an age who is below the age group mentioned in the literature, with no chronic diseases and whose only risk factor is poverty [8-10]. He complained about abdominal pain, nausea, loss of appetite, with a stable clinical condition and no signs of acute infectious disease. However, what really bothered him was the voluminous umbilical protrusion, especially in front of his friends. Because it is an umbilical hernia, we did not request an abdominal CT, although it shows the presence of ascites, calcified lymph nodes with a hypodense center, a thickening of the mesentery, epiploon, peritoneum and adhesions between the intestinal loops, alterations that can be seen in other pathologies [4,10,11].
The preoperative examinations and chest X-Ray of the patient were normal and in view of this clinical condition, we focused only on the umbilical hernia. The patient was referred for surgical treatment.
Through a small incision in the umbilical scar, there was immediately a drainage of ascitic fluid. We chose to enlarge the incision and thus we could detect granulomatous lesions on intestinal loops, appendix, mesentery and peritoneum, which made us think about the possibility of it being peritoneal tuberculosis. In order to elucidate the case and make the differential diagnosis with peritoneal carcinomatosis, we took a sample of the ascitic fluid and performed biopsy of the peritoneum in addition to appendicectomy.
At the same time, laboratory tests were performed to target viral and infectious diseases and PCR for tuberculosis.
The Mycobacteria was not detected in any laboratory tests, corroborating the literature that refers the presence of bacillus in about 3% of cases and in 35% in culture [4,8,10,11].
The identification of Mycobacterium tuberculosis by PCR gen amplification allows a diagnosis of 24 to 48 hours and although it is cited as the ideal test, with a reported sensitivity and specificity of 94% and 88% respectively, there are still limitations, mainly because amplification of bacillus DNA does not always result in live strains, leading to a negative result [10].
In the present case, the diagnosis was only made through peritoneal biopsies, thus confirming the literature reports that refer to a positivity between 85 and 95%, either through laparoscopy or open surgery [4,6,8,10,11].
With the diagnosis of peritoneal tuberculosis confirmed, the patient was discharged from the hospital in good general condition and began specific treatment with the RIPE regimen; in addition, there was a screening for the disease in people with constant contact to assess the existence of other infected individuals.
Conclusion
Tuberculosis is among the top 5 causes of death from infectious disease and the first among infectious disease in HIV-infected patients. It affects the lungs more frequently, although it can also affect the abdomen, involving the digestive and genitourinary tract, abdominal aorta, peritoneum and abdominal lymph nodes, as well as the pleura, bones, lymph nodes and meninges, which are the extrapulmonary tuberculosis group.
Peritoneal involvement represents 0.1 to 0.7% of all types of tuberculosis, with the peritoneum being the 6th most-affected site. Diagnosis of peritoneal tuberculosis is difficult and depends on a high index of suspicion as symptoms are vague and conventional blood and radiological investigations are nonspecific. The identification of Mycobacterium tuberculosis by PCR gene amplification and peritoneal biopsy are ideal tests for diagnosis.
Conflict of Interest
It is stated that there are no conflicts of interest.
References
- Organização Panamericana de saúde (OPAS). Mortes por tuberculose aumentam pela primeira vez em mais de uma década devido à pandemia de COVID-19. [Last accessed on: March 18, 2022] https://www.paho.org
- Secretaria de Vigilância em Saúde Ministério da Saúde. Dados Epidemiológicos da Tuberculose no Brasil. Novembro de 2019. [Last accessed on: March 18, 2022] [email protected]
- World Health Organization – WHO. Global Tuberculosis Report 2021. [Last accessed on: March 18, 2022] https://www.who.int/teams/global-tuberculosis
- Rocha EL, Pedrassa BC, Bormann RL, Kierszenbaum ML, Torres LR, D’Ippolito G. Tuberculose abdominal: uma revisão radiológica com ênfase em achados de tomografia computadorizada e ressonância magnética. Radiol Bras. 2015;48(3):181-91.
- Pareja HBJ, Vidotto JRJr, Cattini MM, Marconi MFA, Gonçalves AL, Goes PAA, et al. Tuberculose Peritoneal, Um Diagnóstico Laparoscópico. Brazilian J Develop. 2021;7(8):77595-601.
- Colósimo AP, Silva AC, Baliello LM, Paula LA, Costa LO, Silva LCL. Tuberculose peritoneal: relato de caso. Rev Méd Minas Gerais. 2006;16(2):112-5.
- Pang Y, An J, Shu W, Huo F, Chu N, Gao M, et al. Epidemiology of extrapulmonary tuberculosis among inpatients, China, 2008-2017. Emerg Infect Dis. 2019;25(3):457-64.
- Fonseca LG, Campos FPF, Felipe-Silva A. Tuberculose peritoneal: experiência em um hospital geral. Autopsy Case Rep. 2011;1(2):3-9.
- Dineen P, Homan WP, Grafe WR. Tuberculous peritonitis: 43 years’ experience in diagnosis and treatment. Ann Surg. 1976;184:717-22.
- Moutinho ACFDF. Tuberculose peritoneal: Um desafio diagnóstico. Tese (Mestrado em Medicina) – Faculdade de Medicina de Lisboa, Portugal. 2006;18.
- Grisi SJFE, Cardoso AC, Bellizia L, Escobar AMU. Tuberculose peritoneal: relato de caso e comparação de métodos diagnósticos. Pediatria (Säo Paulo). 2001;23(1):100-5.
- Lage LP, Chave PMA, Oliveira AA, Peres GGM, Souza LLR, Correia FP, et al. Diagnóstico diferencial entre tuberculose peritoneal e carcinomatose peritoneal. Br J Surg Clin Res. 2018;23(2):66-8.
- Shakil AO, Korula J, Kanel GC, Murray NG, Reynolds TB. Diagnostic features of tuberculous peritonitis in the absence and presence of chronic liver disease: a case control study. Am J Med. 1996;100(2):179-85.
- Al Shohaib S. Tuberculosis in chronic renal failure in Jeddah. J Infect. 2000;40(2):150-3.
- Lui SL, Tang S, Li FK, Li FK, Choy BY, Chan TM, Lo WK, et al. Tuberculosis infection in Chinese patients undergoing continuous ambulatory peritoneal dialysis. Am J Kidney Dis. 2001;38:1055-60.
- Rodriguez E, Pombo F. Peritoneal tuberculosis versus peritoneal carcinomatosis: distinction based on CT findings. J Comput Assist Tomogr 1996;20:269-72.
- Bilgin T, Karabay A, Dolari E, Develioglu OH. Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: A series of 10 cases. Câncer Int J Gynecol. 2001;11:290-4.
- Rabahi MF, Silva Júnior JLR, Ferreira ACG, Tannus-Silva DGS, Conde MB. Tratamento da tuberculose. J Bras Pneumol. 2017;43(5):472-86.
- Comissão Nacional de Incorporação de Tecnologias no Sistema Único de Saúde (CONITEC). [Last accessed on: March 18, 2022] http://conitec.gov.br/ministerio-da-saude
- Ministério da Saúde. Manual de Recomendações para o Controle da Tuberculose no Brasil. 2011. [Last accessed on: March 18, 2022] https://bvsms.saude.gov.br/bvs/publicacoes
- Wismayer R. Abdominal tuberculosis- a resemblance to peritoneal carcinomatosis. J Adv Medicine Med Res. 2021;33(18):87-92.
Article Type
Case Report
Publication History
Received On: 28-02-2022
Accepted On: 17-03-2022
Published On: 24-03-2022
Copyright© 2022 by Garritano C, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Garritano C, et al. A Rare Case of Peritoneal Tuberculosis in a 21 Years Old Male Patient. Surg Res Prac. 2022;3(1):1-9.

Figure 1: Ascitic fluid collected during the surgery.
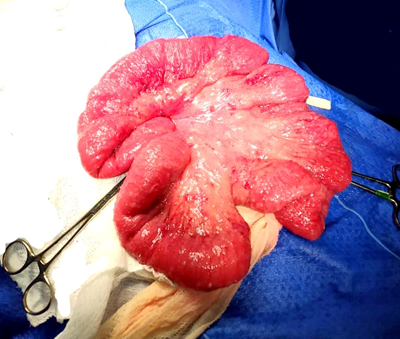
Figure 2: Aspect of jejunal loop.

Figure 3: Aspect of appendix.