Sergey N Gusev1*, Velichko LN2, Bogdanova AV2, Khramenko NI2, Konovalova NV2
1PhD in Medicine and Health Sciences, Author and Owner of Intellectual Property Rights for New Mercureid Molecules, Ukraine
2The Filatov Institute of Eye Diseases and Tissue Therapy of the National Academy of Medical Sciences of Ukraine, Odessa, Ukraine
*Corresponding Author: Sergey N Gusev, PhD in Medicine and Health Sciences, Author and Owner of Intellectual Property Rights for New Mercureid Molecules, Ukraine; Email: [email protected]
Published Date: 26-08-2021
Copyright© 2021 by Gusev SN, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
SARS-CoV-2, the pathogen, which is responsible for coronavirus disease 2019 (COVID-19), has caused unprecedented morbidity and mortality worldwide. Scientific and clinical evidence testifies about long-term COVID-19 effects that can affect many organ systems. Cellular damage, overproduction of proinflammatory cytokines and procoagulant abnormalities caused by SARS-CoV-2 infection may lead to these consequences. After suffering from COVID-19, a negative PCR test is only the beginning of a difficult path to full recovery. 61 % of patients will continue to have the signs of post-covid syndrome with the risk of developing serious COVID-19 health complications for a long time. Post-COVID syndrome is an underestimated large-scale problem that can lead to the collapse of the healthcare system in the nearest future.
The treatment and prevention of post-covid syndrome require integrated rather than organ or disease specific approaches and there is an urgent need to conduct a special research to establish the risk factors.
For this purpose, we studied the expression of markers of apoptosis (CD95) and intercellular adhesion (CD54) in healthy individuals and patients who underwent COVID-19, as well as the efficacy of the drug Mercureid for the treatment of post-covid syndrome.
The expression level of the apoptosis marker CD95 in patients who underwent COVID-19 is 1.7-2.5 times higher than the norm and the intercellular adhesion marker CD54 is 2.9-4.4 times higher. This fact indicates a persistent high level of dysfunctional immune response in the short term after recovery. The severity of the expression of the intercellular adhesion molecule (ICAM-1, CD54) shows the involvement of the endothelium of the vascular wall in the inflammatory process as one of the mechanisms of the pathogenesis of post-covid syndrome.
The use of Mercureid made it possible to reduce the overexpression of CD95 in 73.4 % of patients that led to the restoration of the number of CD4+/CD8+ T-cells, which are crucial in the restoration of functionally active antiviral and antitumor immunity of patients. Also, the use of Mercureid led to a normalization of ICAM-1 (CD54) levels in 75.8 % of patients.
The pharmacological properties of the new targeted immunotherapy drug Mercureid provide new therapeutic opportunities for the physician to influence a number of therapeutic targets, such as CD95, ICAM-1 (CD54), to reduce the risk of post-COVID complications.
Keywords
SARS-COV-2; COVID-19; Coronaviruses; Immunoglobulin
Abbreviations
COVID-19: Coronavirus Disease 2019; SARS-COV-2: Severe Acute Respiratory Syndrome Coronavirus-2; IgG: Immunoglobulin G; VKH: Vogt-Koyanagi-Harada Disease
Introduction
According to the current researches, it is known the following:
- The full range of clinical manifestations of pathologies connected with COVID-19 is not fully examined; new clinical symptoms are still being described.
- Structural and functional changes in organs are still being studied, both as a result of the direct viral effect of COVID-19 and as a result of a violation of homeostasis.
- More and more scientists around the world warn that post-coid syndrome and disorders in the immune status of patients are an underestimated large-scale problem. Cellular damage, a sustained innate immune response with the production of inflammatory cytokines and a procoagulant state caused by SARS-CoV-2 infection lead to these consequences [1-4].
Medicines that are used to treat COVID-19 are also toxic. Long-term use of chloroquine and hydroxychloroquine may result in retinal toxicity. Lopinavir / ritonavir may cause reactivation of autoimmune diseases. Ribavirin causes retinopathy, retinal vein occlusion, serous retinal detachment, non-arterial ischemic optic neuropathy and Vogt-Koyanagi-Harada disease (VKH). Interferon has been connected with retinopathy, conjunctivitis, uveitis, optic neuropathy, corneal ulcers, epithelial defects and Sjogren’s syndrome. Tocilizumab has been reported to cause retinal hemorrhage. Systemic corticosteroids are known to cause cataracts, glaucoma and central serous chorioretinopathy. These points should be taken into account by the physician when prescribing definite treatment for patients [5].
Therefore, the search for new opportunities in the treatment and prevention of complications caused by COVID-19 is undoubtedly an urgent challenge of the time. Our attention was attracted by a new original drug that has no analogues – Mercureid, as a targeted (targeted action) drug aimed at reducing the overexpression of the proinflammatory cytokine TNFα, markers of apoptosis (CD95) and intercellular adhesion ICAM-1 (CD54) and normalization of the production of the most important, if not the main, immunological factor of mucosal immunity, namely, SIgA [6].
According to Swiss molecular biologist Loroch VA (Ph.D in Biology, Experimental research strategies and research methods in molecular genetics and molecular biology, Switzerland) Mercureid’s interaction with the immunoglobulin superfamily changes the paradigm of our thinking about a drug’s mechanism of action, as it leads to many mechanically different biological responses (freely available, link https://vimeo.com/435729749 ):
- Stimulation of secretory Immunoglobulin A. Secretory IgA on the surface of the mucous membrane of the respiratory tract prevents the adhesion of viruses to the surface of the epithelium. Secretory IgA has a non-inflammatory protective function: antibodies of this type can bind to the virus without activating complement and without releasing inflammatory mediators
- Stimulation of neutralizing Immunoglobulin G. Neutralizing IgG prevents the systemic spread of the virus
- Activation of CD4 +, CD8 + and CD16 + T-cells which kill virus-infected cells
- Activation of macrophages. Macrophage-driven phagocytic elimination of cells, which are under apoptosis influence, is an immunologically silent response; there is no inflammation. In fact, it is an anti-inflammatory agent, because macrophages consume apoptotic neutrophils and other cells that produce and secrete pro-inflammatory cytokines as a result of viral infection [7-9]
Thus, we come to the idea that after suffering from COVID-19, a negative PCR test is only the beginning of a difficult path to full recovery and 61 % of patients will continue to have the signs of post-covid syndrome with the risk of developing serious COVID-19 health complications for a long time [10].
Aim of Study
The aim is to study the level of expression of markers of apoptosis (CD 95) and intercellular adhesion ICAM-1 (CD54) in healthy individuals and in patients who underwent COVID-19. In respect that while searching the information in English on the topic: “the level of expression of markers of apoptosis (CD95) and intercellular adhesion ICAM-1 (CD54) in patients who underwent COVID-19” we haven’t found any information available to the public, this immunological study provides a new and extremely important material for practitioners and scientists, allowing for better understanding of the immunopathogenesis of COVID-19.
Material and Methods
This study is open, according to the Declaration of Helsinki on the Moral Regulation of Medical Research, the Convention on Human Rights and Biomedicine developed by the Council of Europe, as well as the relevant laws of Ukraine.
The studies were carried out with the informed consent of patients who were under examination and treatment in the Department of Inflammatory Eye Pathology of the Filatov Institute of Eye Diseases and Tissue Therapy of the National Academy of Medical Sciences of Ukraine. All patients had a history of COVID-19 no earlier than 2-3 months before the medical examination. At the time of treatment and examination, Immunoglobulin M (IgM) was negative for acute coronavirus inflammation. The markers of lymphocyte activation CD95 and ICAM-1 (CD54) were determined by immunohistochemical method in 18 patients (age 43 ± 8 years) at the period of 1-2 months after recovery from COVID-19 and in 27 practically healthy individuals of the control group (age 51 ± 11 years).
Results
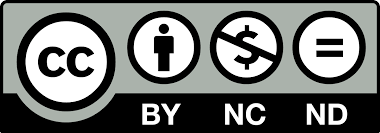
There was a high level of expression of the molecular marker of intercellular adhesion CD 54 on lymphocytes in patients who underwent COVID-19: it was 34.3 ± 5.6% in percentage and 756.13 ± 58.4 cells/μL in absolute value (n = 18). In healthy individuals, these indicators were 2,9,4 times lower (p <0.05 according to the Mann-Whitney U test), respectively that was 12.0 ± 4.0% and 173.5 ± 22.1 cells/μL (n = 22). The level of expression of the molecular marker of apoptosis CD 95 on blood lymphocytes in patients who underwent COVID-19 also exceeded the relative and absolute standard values by 1.7-2.5 times (p <0.05 according to the Mann-Whitney U test), that in relative value it was 31.3 ± 6.8%, in absolute value -660.11 ± 68.4 cells/μL. In general, in healthy individuals, these indicators were 18.2 ± 4.1% and 263.5 ± 32.1 cells/μL, respectively (Fig. 1-4) [11-21].
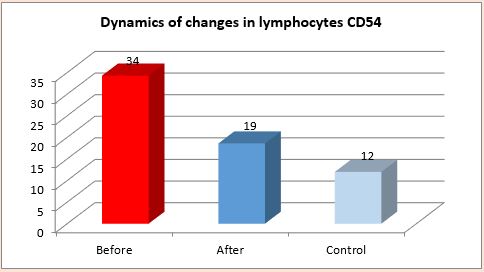
Figure 1: Dynamics of changes CD54 T-cells (before and after taking the medicine Mercureid, in %).
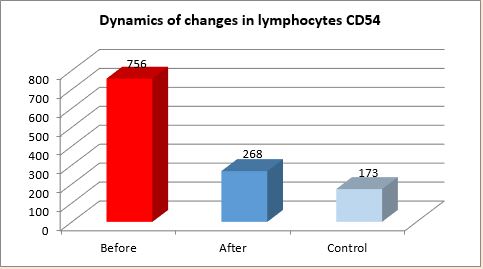
Figure 2: Dynamics of changes CD54 T-cells (before and after taking the medicine Mercureid, in cells/μl).
Figure 3: Dynamics of changes CD95 T-cells (before and after taking the medicine Mercureid, in %).
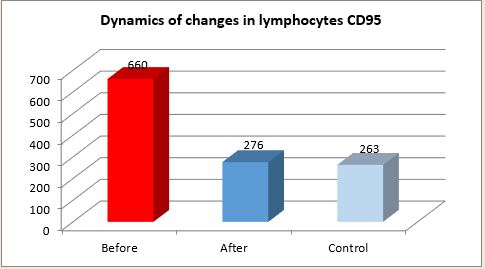
Figure 4: Dynamics of changes CD95 T-cells (before and after taking the medicine Mercureid, in cells/μl).
Conclusion
The expression level of the molecular marker of apoptosis CD95 on blood lymphocytes in patients who underwent COVID-19 is 1.7-2.5 times higher than the norm and the molecular marker of intercellular adhesion CD54 is 2.9-4.4 times higher. This fact indicates a persisting high level of dysfunctional immune response in the short term after recovery.
The severity of the expression of the Intercellular Adhesion Molecule (ICAM-1, CD54) shows the involvement in the inflammatory process the endothelium of the vascular wall as one of the mechanisms of the pathogenesis of post-covid syndrome. Fas (CD95), a cell surface receptor of the tumor necrosis factor superfamily, has long been regarded as a death receptor that mediates apoptosis to maintain immune homeostasis. CD95 is widely expressed in memory T-cells and effector T-cells upon contact with antigen, while naive T-cells are typically negative.
Programmed cell death 1 (PD-1, CD279), effector T-cell antigen, is considered a depletion marker, also expressed during antigen mediated T-cell activation. Upregulation of PD-1 is observed during acute infections and after different viral infections, including HIV, HBV and HCV. In particular, the expression of PD-1 in HIV-specific CD4 + and CD8 + lymphocytes is connected with T-cell depletion and disease progression.
Both antigens are known to be activated upon activation of T-cells and can signal a propensity for apoptosis (CD95) or T-cell depletion (PD-1). We have observed an increased expression of CD95 in T-cells with age that corresponds to the previously described higher susceptibility to CD95-induced apoptosis in the elderly.
Our data on increased expression of CD95, which can induce PD-1 activation, also correspond to the data of Zheng, et al., showing the phenotype of depleted T-cells in patients with severe COVID-19 infection. Apoptosis via CD95 may be a possible mechanism for COVID-19 induced lymphopenia and our data provide new insights into the functional competence of T-lymphocytes in COVID-19 infection.
Aberrant T-cell differentiation and lymphopenia are signs of severe COVID-19 disease. As T-cells must race to discard infected cells, they rapidly differentiate and achieve cytotoxic function. With such reactivity, accelerated apoptosis occurs due to the coupled mechanism of death and differentiation of both CD4 + and CD8 + lymphocytes via CD95 (Fas) and serine threonine kinase (Akt). T-cell lymphopenia in severe cases can mean cell death or peripheral migration. These facets depict SARS-Cov-2 as a lymphatic manipulative pathogen; it distorts T-lymphocyte function, their number and death and creates a dysfunctional immune response.
Thus, we can state that patients who have undergone coronavirus infection are faced with the need to restore immunity. Moreover, the action of the drug should be targeted and directed exclusively at those target proteins that are related to the immunopathogenesis of the development of the disease.
The results after Mercureid application sublingual for 1 month:
- It allowed to reduce the overexpression of CD95 in 73.4% of patients that led to the restoration of the number of CD4 + and CD8 + T-cells, which are crucial in the restoration of functionally active antiviral and antitumor immunity of patients.
- The use of Mercury led to the normalization of the level of ICAM-1 (CD54) in 75.8 % of patients. Recent studies have reported pathological evidence of venous thromboembolism, direct viral infection of endothelial cells and diffuse endothelial inflammation [17]. Therefore, the study of the expression of adhesion molecules ICAM-1 (CD54) of endothelial cells in patients who underwent COVID-19 is of particular value.
Endothelial cells are an important component of the blood coagulation system. Their integrity and functionality are critical for maintaining hemostasis, while damage to endothelial cells from SARS-CoV-2 can lead to platelet activation, thrombosis and inflammation. Dysfunctional endothelial cells activated by proinflammatory cytokines can contribute to the pathogenesis of thrombosis by altering the expression of pro- and antithrombotic factors. In addition, inflammation of endothelial cells causes edema, blockage and thrombosis of small vessels that finally leads to a definite organ ischemia.
Thus, the increased expression of adhesion molecules of endothelial cells is connected with COVID-19 disease, which the patients underwent and it can lead to blood coagulation dysfunction and ischemia development. The use of Mercureid allows not only to have a systemic anti-inflammatory effect, but also to protect the vascular endothelium and reduce the possible risks of thrombosis formation that means the reduction of risks of heart attacks and strokes.
The pharmacological properties of the new targeted immunotherapy drug Mercureid provide new therapeutic opportunities for the doctor to influence a number of therapeutic targets, such as CD95, ICAM-1 (CD54), TNFα to reduce the risk of developing tragic post-covid complications. The treatment should be for a long period of time, about 3-6 months. And in some cases, high-risk patients (diabetes, obesity, autoimmune diseases, hypertension, cerebrovascular disease, elderly age, lung or heart disease) need a lifelong therapy with Mercureid (taking into account its high toxicological safety profile and financial affordability).
Conflicts of Interests
The authors declare that have no competing interest and not any conflict of interest.
References
- Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017-32.
- McElvaney OJ, McEvoy NL, McElvaney OF, Carroll TP, Murphy MP, Dunlea DM, et al. Characterization of the inflammatory response to severe COVID-19 illness. Am J Respir Crit Care Med. 2020;202(6):812-21.
- Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26(5):681-7.
- Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844-7.
- Douglas KA, Douglas VP, Moschos MM. Ocular manifestations of COVID-19 (SARS-CoV-2): a critical review of current literature. In-vivo. 2020;34(3):1619-28.
- Drannik GN, Gorpinchenko II, Kurchenko AI, Gusev SN. Efficacy study of new drug Mercureid (MSC-428) in anti-TNFα therapy for chronic prostatitis. Acta Sci Cancer Biol. 2019;3:9-16.
- Lukyanchuk OV. Results of multitarget therapy anti-PD-1/PD-L1/CD19/CD25/CD38 with application of MSC-428 molecules in patients with different oncopathology. Cancer Biol. 2018;2(10).
- Vladlena G. Dubinina. The results of MSC-428 nanomolecules application in neoadjuvant therapy in patients with breast cancer. J Oncopathol Clin Res. 2019;3(1).
- Velichko LN. Study of the effect of the drug “Mercureid” on the incidence of influenza. Research report department of immunology and pathomorphology the filatov institute of eye diseases and tissue therapy of the national academy of medical sciences of Ukraine. 2016.
- Blomberg B, Mohn KG, Brokstad KA, Zhou F, Linchausen DW, Hansen BA, et al. Long COVID in a prospective cohort of home-isolated patients. Nat Med. 2021;23:1-7.
- Guégan JP, Legembre P. Nonapoptotic function of FAS/CD95 in the immune response. FEBS J. 2018;285:809-27.
- Van den Broek T, Borghans JAM, Van Wijk F. The full spectrum of human naïve T-cells. Nat Rev Immunol. 2018;18:363-73.
- Sharpe AH, Pauken KE. The diverse functions of the PD1 inhibitory pathway. Nat Rev Immunol. 2018;18:153-67.
- Schonrich G, Raftery MJ. The PD-1/PD-L1 axis and virus infections: a delicate balance. Front Cell Infect Microbiol. 2019;13(9):207.
- Phelouzat MA, Laforge T, Arbogat A, Quadri RA, Boutet S, Proust JJ. Susceptibility to apoptosis of T lymphocytes from elderly humans is associated with increased in-vivo expression of functional Fas receptors. Mech Ageing Dev. 1997;96:35-46.
- Zheng HY, Zhang Mi, Yang CX, Zhang N, Wang XC, Yang XP, et al. Elevated exhaustion levels and reduced functional diversity of T-cells in peripheral blood may predict severe progression in COVID-19 patients. Cell Mol Immunol. 2020;17(5):541-3.
- Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417-8.
- Krüger-Genge A, Blocki A, Franke RP, Jung F. Vascular endothelial cell biology: an update. Int J Mol Sci. 2019;20:4411.
- Wong R, Lénárt N, Hill L, Toms L, Coutts G, Martinecz B, et al. Interleukin-1 mediates ischaemic brain injury via distinct actions on endothelial cells and cholinergic neurons. Brain Behav Immun. 2019;76:126-38.
- Fong LY, Ng CT, Zakaria ZA, Baharuldin MT, Arifah AK, Hakim MN, et al. Asiaticoside inhibits TNF-α-induced endothelial hyperpermeability of human aortic endothelial cells. Phytother Res. 2015;29:1501-8.
- Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. The Lancet. 2020;395(10234):1417-8.
Article Type
Research Article
Publication History
Received Date: 26-07-2021
Accepted Date: 18-08-2021
Published Date: 26-08-2021
Copyright© 2021 by Gusev SN, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Gusev SN, et al. Analysis of the Study of the Expression of Apoptosis Markers (CD95) and Intercellular Adhesion Markers (CD54) in Healthy Individuals and Patients Who Underwent COVID-19 When Using the Drug Mercureid. J Clin Immunol Microbiol. 2021;2(2):1-8.
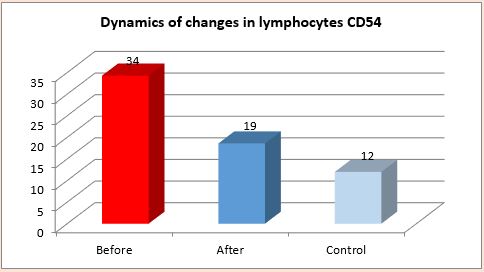
Figure 1: Dynamics of changes CD54 T-cells (before and after taking the medicine Mercureid, in %).
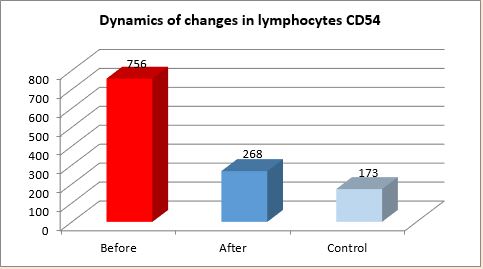
Figure 2: Dynamics of changes CD54 T-cells (before and after taking the medicine Mercureid, in cells/μl).
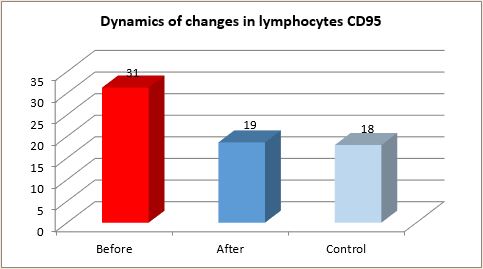
Figure 3: Dynamics of changes CD95 T-cells (before and after taking the medicine Mercureid, in %).
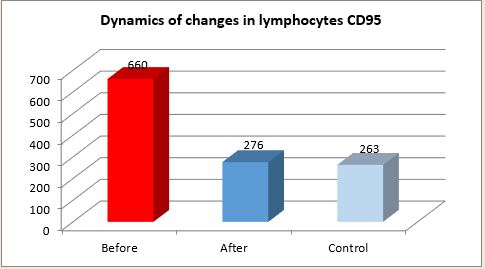
Figure 4: Dynamics of changes CD95 T-cells (before and after taking the medicine Mercureid, in cells/μl).