Clinical Case of a Patient With Aortic Periprosthetic Infection
Lucian-Ion Giubelan1,2, Alexandru Ionuț Neacșu2*, Luiza Cristiana Rǎdoi2, Mirela Mǎnescu2, Eugen Osiac3,4
1Infectious Diseases Department, University of Medicine and Pharmacy of Craiova, Romania
2Hospital of Infectious Diseases and Pulmonology, Craiova, Romania
3Experimental Research Center for Normal and Pathological Aging, Department of Functional Sciences, University of Medicine and Pharmacy of Craiova, Craiova, Romania
4Department of Biophysics, University of Medicine and Pharmacy of Craiova, Craiova, Romania
*Correspondence author: Alexandru Ionuț Neacșu,” Victor Babeș” Hospital of Infectious Diseases and Pulmonology, Craiova, Calea Bucuresti no 126, Craiova, Romania; Email: alex.neacsu1210@gmail.com
Citation: Neacsu AI, et al. Clinical Case of a Patient With Aortic Periprosthetic Infection. Jour Clin Med Res. 2023;4(1):1-4.
Copyright© 2023 by Neacsu AI, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 12 Apr, 2023 | Accepted 07 May, 2023 | Published 14 May, 2023 |
Abstract
Sepsis is the body’s unregulated response to infection and if not properly managed it can lead to septic shock, multiple organ failure and death.
The aim of this article is to present a case of aortic periprosthetic infection, diagnosed in the Infectious Diseases Department of the Hospital no. 3 from Craiova, Romania. Abdominal aortic aneurysm is a serious medical condition, with a high risk of death due to the rupture of the arterial wall. The early antimicrobial treatment decreased the inflammatory markers level Although antibiotic therapy was initiated early, due to multiple associated pathologies, the patient died.
Keywords: Aortic Abscess; Aortic Graft; Periprosthetic Infection; Case Report
Abbreviations
CT: Computed Tomography; ESR: Erythrocytes Sedimentation Rate; G: Gram(S); Iv.: Intravenous; Kg: Kilogram(S); L: Liter(S); M: Meter; Mm3: Cubic Millimetre; MSOF: Multiple System Organ Failure; WBC: White Blood Count
Introduction
Aortic perigraft infection is considered a rare medical condition. Diagnostic guidelines are now in place, however, in spite of prompt antimicrobial therapy and surgical reintervention, mortality remains high. Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection [1]. It is important to be recognized early because often sepsis present as the clinical deterioration of common and preventable infections. If not recognized early and promptly managed, it can lead to septic shock, multiple organ failure and death [2]. The aim of this paper is to present the first case of aortic periprosthetic infection, diagnosed in the Infectious Diseases Department of the Hospital no. 3 from Craiova, Romania. Present study has been approved by the Ethical Committee of the hospital. The patient has signed an informed consent allowing the authors to use his medical data for the purpose of this article.
Case Presentation
The patient PI, male, 72 years old was admitted in the Infectious Diseases Department of the “Victor Babeș” hospital from Craiova on June 17, 2022 for high fever, chills and sharp lumbar pain located on the right abdominal flank. Symptoms started seven days before admission with moderate lumbar pain and low-grade fever, then the complains grew up progressively. Pain and fever killers was given at home as self-medication.
Patient was known with high blood pressure and chronic kidney disease. A computed-tomography scan performed in September 2021 revealed an aortic aneurysm located below the emergence of the renal arteries and up to the bifurcation of the iliac arteries (having a diameter of 65 mm and a length of 81 mm). On April 1st, 2022 he was hospitalized in Bucharest for the cure of an aortic abdominal aneurism rupture and a polyester prosthesis (Polymaille 24 millimetres) was inserted. A retroperitoneal hematoma developed as a complication, however there was a constant medical improvement following the surgical procedure and the patient was discharged in April 19.
When admitted in our hospital he had fever (38.4 Celsius degree), a heart rate of 76 beats/minute, a blood pressure of 114/67 mmHg and his oxygen saturation was 98% while breathing normal air. He had a body-mass index of 23.42 kg/m2 and his general condition was acceptable. He was slightly pale, with a systolic murmur in the aortic area and moderate pain (5 out of 10 on the pain scale) on the middle of the abdomen (particularly around the umbilicus) and the right flank.
The patient’s hemoglobin was 10.5 g/dL (normal range: 12-15), the White Blood Count (WBC) was 22050 cells/mm3 (normal range: 4000-9000) with 83.9% neutrophils on the formula. His erythrocytes sedimentation rate was 80 mm/1 hour (normal range: < 12 mm), the fibrinogen level was 555 mg/dL (normal range: 200-400) and the C reactive protein was detected (120 mg/L, normal range: <10). His blood urine nitrogen level was 52 mg/dL (normal range: 20-40) and the creatinine level was 1.76 mg/dL (normal range: 0.6-1.2). The rest of the investigations were within normal limits.
A Computed-Tomography (CT) scan (performed on June 21) of the abdomen is shown in Fig. 1.
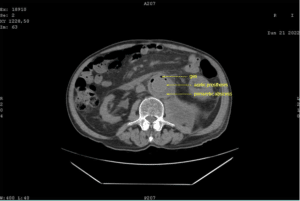
Figure 1: Abdominal CT scan of the patient PI showing the aortic periprosthetic abscess and intra-abdominal hematoma.
Consultation with a cardiovascular surgeon led to the conclusion that an initial antimicrobial treatment is appropriate, followed by a transfer in the cardiovascular clinic. The patient received Ceftriaxone 4 g/day + Linezolid 1.2 g/day + Metronidazole 1 g/day on an Iv. route between admission and until transferred. Under the treatment the white blood cells count dropped to 11270 cells/mm3, but the neutrophils percentage remained high (77.9%). Erythrocytes sedimentation rate and fibrinogen level also went down (55 mm/1 h and 440 mg/dL respectively). Microbiological tests (blood culture and urine culture) were negative. He was transferred in a cardiovascular clinic on June 30. Just before the surgery an Angio CT was performed (Fig. 2).
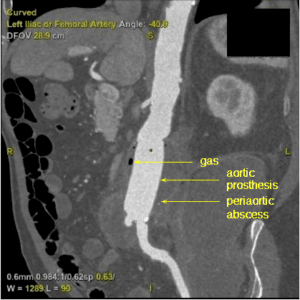
Figure 2: Preparatory Angio CT of the patient PI before vascular surgery.
Following the surgery, the patient developed septic shock and Multiple System Organ Failure (MSOF) and unfortunately, he died two days later. A pus specimen taken from the periprosthetic abscess led to the isolation of Klebsiella pneumoniae (resistant to Piperacillin-Tazobactam, 2nd generation Cephalosporines and Fluoroquinolones).
Discussion
Abdominal aortic aneurysm is a serious medical condition, with a progressive evolution and risk of death due to rupture of the arterial wall. Prevalence of this condition ranges from 1.2 to 6.3%, being the 15th cause of death in elderly from United States [3-5]. The rate of surgical treatment in varies across the world from 2.2 to 17.3 / 100000 habitants considering the elective interventions and 0.5 to 3.3 / 100000 people for the ruptured aneurysms repair [3]. One of the complications of the aortic grafting is infection, with an incidence of 0.5-6% (depending on the surgical procedure used) and an average 30-days mortality of 13.5% (but may be up to 75%) [6,7]. Taking into account the time from implantation there are early and late graft infections, but the threshold between them differs (four months according to European guidelines and two months suggested by the Americans) [8]. Most probably it cannot be a fix limit between those two groups, therefore the presented case is rather an early aortic graft infection. Etiology of aortic graft infections is dominated by Gram positive cocci (Staphylococcus aureus and coagulase-negative staphylococci being isolated in 50-75% of cases), followed by Gram negative bacteria and anaerobes; rare germs or even fungi may also be involved [6,8,9]. When an abscess is involved, from an infectious diseases’ specialist point of view, usually a polymicrobial flora is taken into consideration. Also, the detection of gas formation may suggest the presence of anaerobes. That is the reason for the initial antimicrobial regimen to include a combination of a 3rd generation cephalosporin, oxazolidinones and Metronidazole. The initial microbiological tests were negative, however, pus taken intraoperatory from the periprosthetic abscess led to the isolation of Klebsiella spp., suggesting an intra-abdominal or urinary source of the infection. Diagnostic criteria for the aortic graft infection are presently available [10]. Present case met initially the criteria for suspected case based on a major item (perigraft fluid and gas detection) and two minor criteria (fever and abnormal inflammatory markers, most likely due to an aortic graft infection). Later, the detection of pus around the graft added another major criteria and confirmed the diagnosis. There are defined risk factors contributing to a negative prognosis and the in-hospital mortality increases with the number of the risk factors identified in a certain case [8,9,11]. For the presented case the age of the patient above 70 years, the level of C reactive protein > 50 mg/L are associated with an 85% risk of death [11]; the development of septic shock and MSOF after the surgical intervention also contributed to the infaust prognosis and the decease of the patient.
Conclusion
This is an aortic graft infection due to Klebsiella pneumoniae (the first diagnosed in the “Victor Babeș” Infectious Diseases Clinic from Craiova) treated with a combination of antimicrobials and surgical intervention. However, due to certain risk factors and other underlying conditions and in spite of a decrease of the inflammatory markers level under the antimicrobial treatment, the patient died. This case suggests that early antibiotic therapy is not sufficient to increase the survival rate, and a close collaboration between multiple medical and surgical branch is necessary to increase the survival of patients. A closer look at febrile patients with precordial or abdominal pain and a closer collaboration between different specialists could lead to an earlier diagnosis of aortic infections and a better survival rate.
Authors’ Contribution
LIG and AIN designed the study, collected and analyzed the data, wrote the original draft and approved the final paper. LCR, AIN and LCR analysed the data, critically reviewed the paper. LIG, AIN, LCR and MM approved the final version of the paper.
Conflict of Interest
The authors have no conflict of interest to declare.
References
- Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801-10.
- WHO – Sepsis. [Last accessed on: May 7, 2023] https://www.who.int/news-room/fact-sheets/detail/sepsisf
- Castro-Ferreira R, Lachat M, Schneider PA, Freitas A, Leite-Mereira A, Sampaio SM. Disparities in contemporary treatment rates of abdominal aortic aneurism across Western countries. Eur J Vasc Endovasc Surg. 2019;58(2):200-5.
- Suckow BD, Goodney PP, Columbo JA, Kang R, Stone DH, Cronenwett JL, et al. National trends in open surgical, endovascular and branched/fenestrated endovascular aortic aneurism repair in Medicare patients. J Vasc Surg. 2018;67(6):1690-7.
- Nikol S, Mathias K, Olinic DM, Blinc A, Espinola-Klein C. Aneurysm and dissections – what’s is new in the literature of 2019-2020 – a European Society of Vascular Medicine annual review. Vasa. 2020.
- Post CJHI, Vos CG. Systematic review and meta-analysis on the management of open abdominal aortic graft infections. Eur J Vasc Endovasc Surg. 2019;58:258-81.
- Ge J, Weng C, Zhao J, Yuan D, Huang B, Wang T. Management and clinical outcome of aortic graft infections: a single-center retrospective study. J Clin Med. 2022.
- Van Hemelrijck M, Sromicki J, Husmann L, Rancic Z, Hasse B, Carrel TP. Vascular graft infection. Vessel Plus. 2022.
- Graulus E, Schepens M. Perspective: options in managing aortic graft infections. Indian J Thorac Cardiovasc Surg. 2019;35(2):S186-91.
- Lyons OTA, Baguneid M, Barwick TD, Bell RE, Foster N, Homer-Vanniasinkam S, et al. Diagnosis of aortic graft infection: a case definition by the Management of Aortic Graft Infection Collaboration (MAGIC). Eur J Vasc Endovasc Surg. 2016;52:758-63.
- Garot M, Delannoy PY, Meybeck A, Sarraz-Bournet B, d’Elia PV, d’Escrivan T, et al. Intra-abdominal aortic graft infection: prognostic factors associated with in-hospital mortality. BMC Infect Dis. 2014.
This work is licensed under a Creative Commons Attribution 2.0 International License.


