Correlation of Chest Radiological Findings with Biochemical Markers on Oxygen Requirement in COVID-19 Patients: A Retrospective Analysis
Kamakshi Garg1*, Namrata2, Nitika Singla3, Pratibha DA4, Rajeev Garg5, Devinderpal Singh Dhanota6, Kavita Saggar7
1Professor, Department of Anesthesiology, Dayanand Medical College and Hospital (DMCH), Ludhiana, India
2Associate Professor, Department of Anesthesiology, Dayanand Medical College and Hospital (DMCH), Ludhiana, India
3Senior Resident, Department of Critical Care Medicine, BL Kapoor Hospital, New Delhi, India
4Senior Resident, Department of Anesthesia, Employees State Insurance Hospital (ESI), Ludhiana, India
5Senior Consultant and Director in Radiodiagnosis, Rednet diagnostics, Ludhiana, India
6Assistant Professor, Department of Radiodiagnosis, Dayanand Medical College and Hospital (DMCH), Ludhiana, India
7Professor and Head, Department of Radiodiagnosis, Dayanand Medical College and Hospital (DMCH), Ludhiana, India
*Corresponding Author: Dr Kamakshi Garg, Professor, Department of Anesthesiology, Dayanand Medical College and Hospital (DMCH), Ludhiana, India; Email: drkamakshigarg@gmail.com
Citation: Garg K, et al. Correlation of Chest Radiological Findings with Biochemical Markers on Oxygen Requirement in COVID 19 Patients: A Retrospective Analysis. Jour Clin Med Res. 2022;3(2):1-11.
Copyright© 2022 by Garg K, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 08 Apr, 2022 | Accepted 29 Apr, 2022 | Published 06 May, 2022 |
Abstract
Background: The study is to correlate Chest X-ray scoring with the laboratory markers and to determine the oxygen requirement in COVID-19 patients.
Methodology: We conducted a retrospective study in COVID confirmed patients in the age group of 18 to 80 years admitted in our health care system. At the time of admission within 24 hours, chest X-ray and blood investigations like complete blood count, C-reactive protein, Lactate Dehydrogenase (LDH), d-dimers, serum ferritin were performed in all the patients. Patients data including his oxygen requirement was collected by electronic medical records. Brixia scoring system was employed to account for the extent and density of airspace opacification. The scoring of the Chest X-ray was correlated to the various blood test.
Result: One hundred nine COVID confirmed cases were included in our study. There was a statistically significant correlation between Chest X-ray and age with p = 0.008; chest X-ray and d-dimers with p=0.004. Also patients requiring high oxygen therapy had significantly higher chest X-ray scores (p=0.001)
Conclusion: Patient having increased oxygen requirement were found to have higher N/L Ratio, D-dimer and LDH values. Chest X-ray scoring is highly correlated with laboratory findings and disease severity and might be beneficial to speed up the diagnostic workflow in symptomatic patients.
Keywords
COVID-19; Chest X Ray; D-Dimer; C-Reactive; Serum Ferritin; Lactate Dehydrogenase
Introduction
Coronavirus disease 2019 (COVID-19) was declared a global pandemic and a public health emergency by WHO as it created havoc in terms of morbidity and mortality in India. The clinical features usually range from a mild common cold-like illness, to a severe viral pneumonia leading to acute respiratory distress syndrome that is potentially fatal [1]. Majority of the patients develop mild symptoms such as fever, dry cough, fatigue and shortness of breath, approximately 10% of the patients required hospitalization. Among the hospitalized individuals, around 10% of them required intensive care including invasive ventilation for Acute Respiratory Distress Syndrome (ARDS). Although a confirmed diagnosis of COVID-19 requires PCR identification of viral nucleic acid but chest X-ray imaging also played a very important role to detect the extent of disease.
Chest X-ray is an easily available bed side imaging modality to evaluate any respiratory illness and hence forms the first imaging modality of choice in COVID-19 [2]. Although CT scan was presumed to be more accurate to diagnose COVID-19 with a sensitivity of 83.3% and specificity of 94%, the major limitation to this modality is availability and transportation of the COVID-19 patients. Hence chest X-ray plays a major role in the initial evaluation and follow-up of these patients. Currently there are two different chest X-ray scoring systems such as Radiographic Assessment of Lung Edema (RALE) and Brixia scoring used in staging the severity of COVID-19 infection. Brixia scoring system is widely used to monitor the severity and progression of the disease [3].
Various studies conducted on chest X-ray evaluation found lower sensitivity for COVID-19 related lung opacification (25 to 69%); however, specificity is high around 90 % [4]. Despite lower sensitivity with regards to CT scan, the American College of Radiology and Fleischner Society both endorse the use of Chest X-rays because of its easy portability and early sanitisation as compared to CT scan for COVID-19 [4,5]. Given that our battle against COVID-19 may be long drawn, it is imperative that we define the role of chest X-ray and also its diagnostic performance by comparing it with the commonly used blood markers.
The immunological, inflammatory and coagulative cascades are closely interlinked and hence a strong working knowledge of pathophysiology is required to identify biomarkers that can predict the severity of the disease and response to therapy [6]. Estimation of various blood markers such as C-reactive protein, D-dimer, lactate dehydrogenase and ferritin are routinely performed to support the clinical decision making and timely management of the patients. These tests are useful in assessing the severity of the disease and predict complications such as Disseminated Intravascular Coagulation (DIC) and multiple organ failure in these patients to detect the level of inflammatory process going inside the body [7]. The purpose of this study was to evaluate the severity of COVID-19 infection by quantifying chest X-ray results and to determine the relationship between chest X-ray score and systemic inflammatory mediators so as to identify factors which can be used for COVID-19 pandemic.
Material and Methods
This was a retrospective observation study conducted in confirmed COVID-19 patients admitted to a tertiary care centre from May 2020 to August 2020 following approval from Institutional Ethics Committee.
A total number of 219 patients presented to our hospital between May-August 2020, out of which 146 patients were tested RT-PCR positive for COVID-19. Among them data of 37 patients were excluded due to missing data records. Finally, a total number of 109 patients were analysed in the present study. Baseline laboratory investigations such as complete blood count, renal and liver function tests, C-reactive protein, lactate dehydrogenase, D-dimer and chest X-ray were collected. These blood investigations and chest X-ray were repeated at intervals to monitor disease progression. Patient demographic data and clinical profile such as date of hospital admission, age, gender, smoking history, relevant clinical features like body temperature, oxygen saturation and details of oxygen therapy were collected from electronic medical record.
Empiric broad spectrum antibiotics and remdesivir were prescribed for suspected community acquired pneumonia, which were ceased if no bacterial cause or influenza was detected. In the absence of any effective antivirals, treatment was largely supportive with supplemental oxygen administered if oxygen saturation by pulse oximetry was ≤ 94%.
Chest X-ray was done in all RT-PCR positive patients on first day of admission using portable digital radiography system. All CXR images, including portable CXR, were acquired on digital radiography units, and exported from Picture Archiving and Communication System in Digital Imaging and Communications in Medicine format in an anonymized format. Each frontal chest projection was independently reviewed by a radiologist with 15 years’ experience of thoracic imaging, using the Brixia score system. The radiologist were blinded in their review from the subjects’ clinical outcome and the CXRs were randomised. CXRs which were technically suboptimal were highlighted by our radiologists and excluded.
Each lung was divided into three zones, named from A to F; upper (A/D) above aortic arch to hilum, middle zones (B/E) below aortic arch to hilum and lower zones (C/F) below hilum to bases, on both postero-anterior and antero-posterior projection.
Each zone was given a score of 0 to 3 based on lung abnormality detected: score 0 corresponding to no abnormality; score 1- interstitial infiltrates; score 2- interstitial and alveolar infiltrates with interstitial predominance; score 3- interstitial and alveolar infiltrates with alveolar predominance [8].
Scores were added to form a cumulative chest X-ray score ranging from 0 to 18, with partial score of each zone entered as well. Other additional finding such as pleural effusion were mentioned separately. Chest X-ray scores were categorised into mild, moderate and severe with score of <5, 5-10, >10 respectively.
We also classified the patient on terms of oxygen requirement i.e low FiO2 (patient on room air, binasal, venturi) and high FiO2 (i.e NRBM, Airvo, NIV)
We also compared initial chest X-ray score with oxygen requirement, biochemical markers and demographic data.
Statistical Analysis
Data were described in terms of range; mean ± Standard Deviation (± SD), frequencies (number of cases) and relative frequencies (percentages) as appropriate. Comparison of quantitative variables between the study groups was done using ANOVA. For comparing categorical data, Chi square (χ2) test was performed and exact test was used when the expected frequency is less than 5. Pearson Correlation was used. A probability value (p-value) less than 0.05 was considered statistically significant. All statistical calculations were done using (Statistical Package for the Social Science) SPSS 21version (SPSS Inc., Chicago, IL, USA) statistical program for Microsoft Windows.
Results
A total number of 219 patients presented to our hospital with complaints of fever and shortness of breath, out of which 146 patients were tested RT-PCR positive for COVID-19. Among them data of 37 patients were excluded due to missing data records. Finally, a total number of 109 patients were analysed in the present study.
The mean age of the patients was 58.7 years. Seventy four had comorbidities in the form of diabetes, hypertension, coronary artery disease and cardiovascular accidents. The most common co-morbid condition associated was diabetes mellitus in 51% patients followed by hypertension in 37.6% patients. The average oxygen saturation on room air at admission was 86%. About 35.78% patients required low flow oxygen therapy while 34.8% patients required high flow oxygen therapy (Table 1).
Baseline X-ray was performed in all patients at the time of admission and graded according to Brixia Scoring system. Patients were classified based on the scores. There were 32 patients with score <5; 55 patients with score 5-10 and 22 patients with score >10 (Table 2). High flow oxygen requirement was 6.25% patients with Brixia score <5; 40% patients with Brixia score 5-10; 63.64% patients with score > 10. This was statistically significant. Overall, patients on low flow oxygen therapy (35.78%) had significanltly lower scores on chest X-ray (p= 0.001), while patients on high flow oxygen therapy (34.8%) had significantly higher scores (p= 0.001) (Table 3).
Association between Biochemical markers and oxygen therapy: Baseline biochemical markers such as LDH, D-dimer, CRP and N/L ratio were noted on Day 1 of admission. Patients requiring high flow oxygen therapy had significantly higher LDH (p= 0.001), D-dimer (0.007) and N/L ratio (p= 0.05). While serum ferritin and CRP were also higher in patients requiring high flow oxygen therapy, they were not statistically significant (Table 4,5).
Correlation between chest X-ray and biochemical markers along with demographic data (Fig. 1):
There was a significant correlation between age and CXR scoring (r= 0.25, p=0.008). Significant correlation was also noted with D-dimer (r= 0.27, p= 0.004). Although a positive correlation was noted it was not statistically significant with N/L ratio (r= 0.12, p= 0.2), CRP (r=0.11, p= 0.23) and LDH (r= 0.14, p= 0.12).
No. of cases | %age | ||
Age | < 50 | 22 | 20.18% |
51-70 | 70 | 64.22% | |
> 70 | 17 | 15.60% | |
Oxygen Requirement | Low flow | 39 | 35.78% |
Room air | 32 | 29.36% | |
High Flow | 38 | 34.86% | |
Diabetes | Yes | 56 | 51.38% |
No | 53 | 48.62% | |
Hypertension | Yes | 41 | 37.61% |
No | 68 | 62.39% |
Table 1: Distribution of patients in terms of age, oxygen requirement and co-morbidities.
Chest X-ray Brixia Scoring Group | Total | Chi-square value | p-value | ||||
< 5 | 5-10.0 | >10 | |||||
Age | < 50 | 11 | 9 | 2 | 22 | 6.946 | 0.139 |
51-60 | 11 | 19 | 8 | 38 | |||
> 60 | 10 | 27 | 12 | 49 | |||
Total | 32 | 55 | 22 | 109 | |||
Table 2: Correlation of age with Brixia Scoring System.
Chest X-ray Scoring Group | Total | Chi-square value | p-value | |||||||
< 5 | 5-10.0 | >10 | ||||||||
Oxygen Requirement | Low flow | 12 | 37.50% | 20 | 36.36% | 7 | 31.82% | 39 | 26.394 | 0.0001 |
Room air | 18 | 56.25% | 13 | 23.64% | 1 | 4.55% | 32 | |||
High Flow | 2 | 6.25% | 22 | 40.00% | 14 | 63.64% | 38 | |||
Table 3: Chest X-ray scoring.
Low flow | High flow | Z | p-value | |||
Mean | SD | Mean | SD | |||
AGE | 57.23 | 11.95 | 61.08 | 12.32 | -1.587 | 0.115 |
N/L ratio | 9.78 | 11.22 | 15.22 | 17.27 | -1.986 | 0.05 |
DDIMER | 561.73 | 354.77 | 741.66 | 257.12 | -2.76 | 0.007 |
CRP | 125.97 | 183.87 | 136.92 | 101.65 | -0.34 | 0.735 |
FERRITIN | 729.48 | 844.84 | 709.39 | 620.49 | 0.129 | 0.898 |
LDH | 321.12 | 139.38 | 523.08 | 431.29 | -3.62 | 0.001 |
Table 4: Chest X-ray scoring mean and standard deviation analysis.
AGE | E | DDIMER | CRP | FERRITIN | LDH | ||
Chest X-ray Scoring | Pearson Correlation | 0.254 | 0.122 | 0.277 | 0.116 | -0.108 | 0.147 |
p-value | 0.008 | 0.207 | 0.004 | 0.23 | 0.265 | 0.128 | |
N | 109 | 109 | 109 | 109 | 109 | 109 |
Table 5: Chest X-ray scoring different analysis.
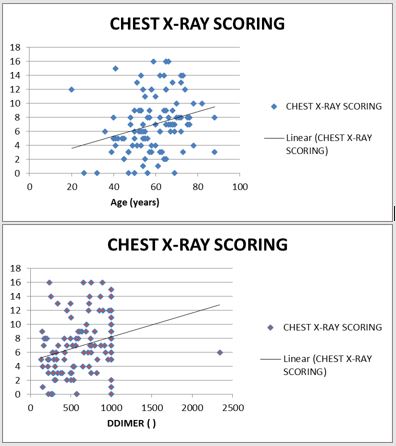
Figure 1: Chest X-ray scoring.
Discussion
The clinical value of Chest X-rays for COVID-19 infectious disease has always remained explicated. Studies have found the extent of lung involvement in CT imaging are more accurate in identifying the severity of COVID-19 infection and can also predict the ICU admission or death. CT imaging is however reserved for those patients in whom other underlying etiologies, such as pulmonary embolism need to be excluded [9].
SARS CoV-2 is a highly contagious virus in which transmission occurs even via asymptomatic patients during incubation period. Exponential rise in the number of the cases has created a great challenge. This virus mainly affects respiratory system leading to cough, dyspnea, fatigue, respiratory failure [10]. Early diagnosis and treatment of the disease affects the morbidity and mortality in these patients.
Earlier studies have revealed that chest X-ray exhibits distinct visual characteristics. This has made radiology a forefront speciality during the outbreak of COVID-19. Though the current literature suggests the potential role of CT scan in diagnosing as well as predicting the outcome of the SARS CoV-2 patients but this creates a huge burden on the radiologists [11]. Chest X-rays are more cost effective, less time consuming and does not require transportation of the patient which is a major limiting factor for CT scan in COVID-19 patients. All this makes chest X-ray a better substitute to CT scan.
The limited sensitivity of CT scan for patients is further stressed by Xu, et al., who studied a cluster of asymptomatic or mildly symptomatic COVID-19 patients with negative CT findings [12]. Though chest X-ray is less sensitive for diagnosis but serial chest X-rays do help in monitoring the disease progression. A retrospective study done by Hyunjoong W Kim evaluated the usefulness of chest X-ray for triaging patients with higher degree of alveolar opacities. They found that increasing severity of alveolar opacities on chest X-ray was associated with increasing age. Also, lower oxygen saturation and higher degree of alveolar opacities in initial chest X-ray were associated with significantly increased duration of hospitalization and increased likelihood of intubation (0.004) [13]. In our study, we also observed a significant increase in alveolar opacities as per Brixia scoring in older patients as compared to young patients (p-value-0.008). This could be explained by increase in co-morbid conditions in older patients and suppression of immune system.
We correlated chest X-ray scoring with the biochemical markers for the need of oxygen supplementation in COVID-19 confirmed cases. Previous studies have compared the correlation of CRP, LDH, D-dimer, lower lymphocyte count with the chest X-ray scoring. They were of the opinion that patients requiring oxygen supplementation were of increased age with associated comorbidities. These patients had significantly higher CRP, higher LDH and lower lymphocyte count along with a positive correlation with the chest X-ray [8,9]. In our study, we analysed chest X-ray finding using BRIXIA score on the first day of admission in COVID-19 confirmed cases. We correlated this initial chest X-ray score with the biochemical markers like CRP, LDH, D-DIMER, neutrophil to lymphocyte ratio and ferritin on the same day. Higher values of D-dimer, LDH, CRP and N:L ratio have been observed in patients having higher Brixia score. A statistically significant correlation between chest Xray scores and D-dimer was found (p-value- 0.004) in our study.
A study reported that an elevated plasma levels of Fibrin degraded products including D-dimer is a significant independent biomarker of poor prognosis. Severe COVID-19 pnuemonia is associated with widespread activation of coagulation system leading to increased levels in APTT, PT and D-dimer levels resulting in higher incidence of pulmonary and peripheral venous thrombosis, stroke and acute coronary syndromes. The development of microthrombi in pulmonary capillaries explains the profound hypoxia in these COVID-19 patients. Activation of coagulation system is known to be pro-inflammatory which drives further inflammation in delicate tissue such as lung causing impaired gas exchange that can be highly detrimental and leads to ARDS [14]. Zhou and co-authors showed that 68% of patients with COVID-19 had increased coagulation as shown by increased D-dimer levels (0.5ug/ml) [15].
Chest X-ray was also compared with the oxygen requirement in our study. We found that the patient having higher Brixia score on radiographs required a statistically significant high flow of oxygen therapy (p-value- 0.0001). This implicates the need for CXR to be performed routinely for follow-up of the patients which allows for swift recognition in the progression of the disease and guide the therapy.
Terrence, et al., studied 109 patients out of which 8 needed supplemental oxygen. The authors reported that patients requiring supplemental oxygen had higher CRP, LDH and lower lymphocytic count (p<0.001) along with a higher CRS score [9]. Another study conducted by Sean Wei, et al., among 109 COVID-19 confirmed patients found that group of patients with high risk chest X-ray findings also had significantly greater odds of requiring supplemental oxygen which is in contiguity with our study. They were also significantly older and had various comorbidities. Higher scores on chest X-ray was also associated with significantly low lymphocyte count, high CRP and high LDH level [16].
Our study found statistically significant correlation between biochemical biomarkers like N/L ratio, D-dimer, LDH with the oxygen requirement on the day of admission. Patient having increased oxygen requirement were found to have higher N/L Ratio, D-dimer and LDH values. This necessitates a need for measuring these biochemical markers along with chest X-ray at regular intervals when monitoring the course of disease and to categorize the severity of patients accordingly.
There are several limitations of our study. (1) It was a retrospective study. (2) We did not study relationship between chest X-ray and length of the stay of patients. (3) We compared chest X-ray on the first day of admission with biochemical markers irrespective of number of days of illness. (4)The temporal profile of chest X-ray and bio-chemical markers were not followed over the disease course. (5) We did not follow up the patient for the entire course of illness.
Conclusion
Patient having increased oxygen requirement were found to have higher N/L Ratio, D-dimer and LDH values. Chest X-ray scoring is highly correlated with laboratory findings and disease severity and might be beneficial to speed up the diagnostic workflow in symptomatic patients.
Conflict of Interest
The authors declare no conflict of interest.
References
- Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020;45(8):100618.
- Chandra TB, Verma K, Singh BK, Jain D, Netam SS. Coronavirus disease (COVID-19) detection in chest X-Ray images using majority voting based classifier ensemble. Expert Syst Appl. 2021;165:113909.
- Setiawati R, Widyoningroem A, Handarini T. Modified chest X-Ray scoring system in evaluating severity of COVID-19 Patient in Dr. Soetomo general hospital surabaya, Indonesia. Int J Gen Med. 2021;14:2407-12.
- Choi H, Qi X, Yoon SH, Park SJ, Lee KH, Kim JY, et al. Extension of coronavirus disease 2019 (COVID-19) on chest CT and implications for chest radiograph interpretation. Radiology: Cardiothoracic Imaging. 2020;2(2):e200107.
- Wong HY, Lam HY, Fong AH, Leung ST, Chin TW, Lo CS, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2020:201160.
- Gemcioglu E, Davutoglu M, Catalbas R, Karabuga B, Kaptan E, Aypak A, et al. Predictive values of biochemical markers as early indicators for severe COVID-19 cases in admission. Future Virol. 2021;16(5):353-67.
- Letelier P, Encina N, Morales P, Riffo A, Silva H, Riquelme I, et al. Role of biochemical markers in the monitoring of COVID-19 patients. J Med Biochem. 2021;40(2):115-28.
- Monaco CG, Zaottini F, Schiaffino S, Villa A, Della Pepa G, Carbonaro LA, et al. Chest X-ray severity score in COVID-19 patients on emergency department admission: a two-centre study. Eur Radiol Exp. 2020;15;4(1):68.
- Hui TCH, Khoo HW, Young BE, Haja Mohideen SM, Lee YS, Lim CJ, et al. Clinical utility of chest radiography for severe COVID-19. Quant Imaging Med Surg. 2020;10(7):1540-50.
- Zhang J, Meng G, Li W. Relationship of chest CT score with clinical characteristics of 108 patients hospitalized with COVID-19 in Wuhan, China. Respir Res. 2020;21:180.
- Yasin R, Gouda W. Chest X-ray findings monitoring COVID-19 disease course and severity. Egypt J Radiol Nuclear Med. 2020;51(1):193.
- Xu R, Du M, Li L, Zhen Z, Wang H, Hu X. CT imaging of one extended family cluster of corona virus disease 2019 (COVID-19) including adolescent patients and “silent infection”. Quant Imaging Med Surg 2020;10:800-4.
- Kim HW, Capaccione KM, Li G. The role of initial chest X-ray in triaging patients with suspected COVID-19 during the pandemic. Emerg Radiol. 2020;27(6):617-21.
- José RJ, Williams A, Manuel A, Brown JS, Chambers RC. Targeting coagulation activation in severe COVID-19 pneumonia: lessons from bacterial pneumonia and sepsis. Eur Respir Rev. 2020; 29(157):200240.
- Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-62.
- Ong SWX, Hui TCH, Lee YS, Haja Mohideen SM, Young BE, Tan CH, et al. High-risk chest radiographic features associated with COVID-19 disease severity. PLoS One. 2021;16(1):e0245518.
This work is licensed under Attribution-NonCommercial-NoDerivs 2.0 Generic (CC BY-NC-ND 2.0) International License. With this license readers are free to share, copy and redistribute the material in any medium or format as long as the original source is properly cited.

