Effect of Early Administration of Oropharyngeal Colostrum in Reducing Late Onset Neonatal Sepsis
Md Abdul Mannan1*, Shazia Afreen2, Md Nazmus Sihan3, Sadeka Choudhury Moni4, Ismat Jahan5, Rumpa Mani Chowdhury6, Kamrul Hassan Shabuj7, Md Shahidulla8
1Professor of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
2Resident of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3Resident Physician (Paediatrics), Cumilla Medical College Hospital, Cumilla, Bangladesh
4Assistant Professor of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
5Assistant Professor of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
6Assistant Professor of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
7Assistant Professor of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
8Professor of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
*Correspondence author: Md Abdul Mannan, Professor, Department of Neonatology, Bangabandhu Sheikh Mujib Medical University, Bangladesh; Email: drmannan64@gmail.com
Citation: Mannan AM, et al. Effect of Early Administration of Oropharyngeal Colostrum in Reducing Late Onset Neonatal Sepsis. Jour Clin Med Res. 2023;2(1):1-8.
Copyright© 2023 by Mannan AM, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 04 Apr, 2023 | Accepted 17 Apr, 2023 | Published 25 Apr, 2023 |
Abstract
Background: Early administration of colostrum by oropharyngeal route plays a tremendous role in preventing mortality and morbidity in preterm infants. The objective of this study was to determine if oropharyngeal administration of mother’s own colostrum within 24 hrs of life can reduce rates of Late Onset Neonatal Sepsis (LONS) in preterm neonates.
Methods: This randomized, placebo-controlled study was conducted in the Department of Neonatology, Bangabandhu Sheikh Mujib Medical University, Dhaka from July, 2019 to June, 2021. Neonates with birth weight ≤ 1800 g and/or gestational age ≤ 34 weeks were enrolled in this study. Intervention group received maternal colostrum (0.2 mL), within 24 hours of birth, every 3 hrly for the next 3 days. Serum IgA was measured at 24hrs and 7th day of postnatal age.
Results: A total of 104 neonates were enrolled, 52 were randomized to oropharyngeal administration of colostrum group and 52 to placebo group. Finally, 40 patients among the placebo group completed the study. There was reduction in the incidence of LONS 55.7% vs. 85% (p = 0.003); probable sepsis 46.1% vs. 70% (p = 0.033), proven sepsis 36.5% vs. 57.5% (p = 0.058). Among the secondary outcome there was reduction of DIC 23% vs. 55% (p = 0.002), use of mechanical ventilators 21.1% vs 55% (p = 0.001), no of inotropes 1.18±0.395 vs 1.61±0.497 (p = 0.002), duration of inotropes 19.77±14.249 vs. 36.57±17.502; (p = 0.002).
Conclusion: This study concluded that the incidence of late-onset neonatal sepsis, DIC, use of MV and inotropes, duration of inotropes can be significantly reduced in preterm neonates by oropharyngeal administration of mother’s own colostrum.
Keywords: Oropharyngeal Administration; Colostrum; Preterm; Late Onset Neonatal Sepsis; RCT
Introduction
Fifteen million babies are born preterm every year and the trend is rising. The leading cause of death among children under 5 years is complications related to preterm birth, which is responsible for approximately 1 million deaths in 2015 [1]. Despite improvement in neonatal care and treatment modality, mortality and morbidity remain high in this population [1,2]. Late-Onset Neonatal Sepsis (LONS), defined as a microbial infection evident by positive blood culture after 72 hours of life is associated with a high burden of morbidity and mortality in preterm infants [3]. Sepsis and NEC, are associated with poor growth and neurodevelopmental outcomes [4]. Preterm neonates are at increased risk of sepsis and NEC despite of variety of infection control measures. These morbidities also lead to prolonged hospital stays and increases in the cost of care [5,6]. The exposure of the growth and protective biofactors of the amniotic fluid during fetal life can be continued and enhanced by colostrum, the fluid secreted by the mammary glands in the first few postnatal days, is rich in biological protective factors, present in a higher concentration in the colostrum of mothers who have delivered preterm infants. Colostrum may act via different mechanisms: as a local barrier that prevents adhesion of microbes to the mucosa, modulating cytokine interaction with oropharyngeal mucosa associated lymphoid tissues, facilitating the absorption of immune factors by the buccal mucosa. Other beneficial factors of colostrum are its prebiotic and anti-inflammatory actions, antioxidant properties of lactoferrin and by the stimulation of intestinal growth and repair [7]. Similarly, to being absorbed by using the intestinal tract, those immunoactive elements also can produce specific advantages through oropharyngeal contact by using “according to oral breast milk feed”, which might also sell immunocompetence via mechanisms of immunomodulation of cells inside the Oropharyngeal-Related Lymphoid Tissue (OFALT) and Intestine-Related Lymphoid Tissue (GALT) systems, and the mucosal absorption of things that intervene with bacterial colonization. Because of bad sucking swallowing coordination and medical instability preterm neonates with GA <34 weeks fed via a nasogastric tube (breast milk cannot pass via the oropharynx) inside the early postnatal days. This contributes to danger of sepsis because of the absence of oropharyngeal publicity to immunoactive elements in the course of this critical period [8]. Transforming Growth Factor-β (TGF-β) is an anti-inflammatory cytokine found in human colostrum. TGF-β is also responsible for the antibodies produced by B-lymphocytes’ class-switching, in particular, secretory Immunoglobulin A (IgA). Japanese researchers found a correlation between the TGF-β1 concentration in human milk and IgA levels in the infant serum IgA secretion in human milk is vital to provide passive immune protection, as the newborn infant is unable to synthesize antibodies until 30 days postpartum. Serum IgA was measured in blood to evaluate the production of bioactive proteins after activation of oropharyngeal Mucosa-Associated Lymphoid Tissue (MALT). To date there are no available data regarding protective role of buccal colostrum on preventing LONS in Bangladesh. The objective of this study was to determine if oropharyngeal administration of mother’s own colostrum within 24 hrs of life can reduce rates of Late Onset Neonatal Sepsis (LONS) in preterm neonates.
Materials and Methodology
Study design: This randomized, placebo-controlled study was done in the Department of Neonatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Shahbag, Dhaka, Bangladesh from July 2019 to June 2021, after getting the approval from the Institutional Review Board.
Eligibility criteria’s: All inborn preterm neonates gestational age <34 weeks and birth weight ≤1800 g for whom parenteral consent obtained were eligible for enrollment. Infants with gross congenital anomalies, any surgical condition where there is contraindication of breast milk, newborn who died within 7 days, were excluded from the study.
Data collection procedures: Face-to-face interview with the mother or caregivers were taken for all enrolled neonates. Information regarding demographic and socioeconomic status was recorded. After informed parental consent, each neonate was randomly assigned by computer generated random number either to the colostrum or standard care group. Attending physicians decided the feeding status of each neonate. Within 24 hours of delivery mothers of each neonate of colostrum group was met by investigators and educated about hand-expression and pumping of breast milk every 2 to 3 hrs. Mothers were instructed to collect their colostrum in a prelabelled sterile container by using a hand-expression method and then to send the colostrum to the NICU. One ml disposable syringes were used to administer colostrum via the oropharyngeal route. Within 24 hrs of birth, each neonate of colostrum group received 0.2 mL of his or her mother’s colostrum (0.1 ml in each buccal mucosa) every 3 hrs for 72 consecutive hours, regardless of whether the infant was fed enterally. The colostrum was administered toward the posterior oropharynx for at least 10 seconds by placing one ml syringe containing 0.1 ml of colostrum on patient’s each buccal mucosa. Vital parameters such as Heart Rate (HR), Respiratory Rate (RR), blood pressure, and pulse oxygen saturation (SpO2) was recorded immediately before and after every intervention session. If there was a requirement of an increase in fraction of inspiratory oxygen 0.1 to maintain SpO2 between 90-95%, bradycardia (HR<100/minute) or tachycardia (HR 200/minute), and tachypnea (RR 80/minute) then session was planned to discontinue. Placebo group received normal saline in buccal mucosa 0.2 ml 3 hrly for 72 hrs.
Serum IgA was measured before applying colostrum and placebo as normal saline and at 7th day of age in colostrum and placebo group respectively. Data from history, physical examination and investigations were recorded in predesigned questionnaire. Maternal data including number of fetuses, use of antenatal corticosteroids, antenatal antibiotics and presence of PROM were recorded. Newborn’s clinical data including gestational age, birth weight, Apgar score, weight and postnatal age at the onset of sepsis, heart rate, blood pressure, CRT, temperature were also recorded. Biological and bacteriologic data were also collected that included blood cell count, CRP, heper or hypo glycaemia and pathogen. The incidence of LONS, and other comorbidities of prematurity, such as Bronchopulmonary Dysplasia (BPD), Ventilator-Associated Pneumonia (VAP), Retinopathy of Prematurity (ROP), Intraventricular Haemorrhage (IVH), clinical, probable and proven sepsis and mortality were documented. Following data were recorded at the time of discharge or death: duration of NICU stay, duration of mechanical ventilation, number and duration of inotropes/vasopressor required. Primary outcome variables were LONS, survival rate, serum IgA level at 1st and 7th day. Sepsis that developed after 72 hrs of postnatal age was defined as Late onset neonatal Clinical sepsis was defined as clinical signs of infection without any laboratory evidence of sepsis accompanied by concurrent antibiotic treatment for 3 days. Probable Sepsis was defined as presence of signs and symptoms of infection along with at least two abnormal laboratory results when blood culture is negative. Proven sepsis was defined as clinical picture suggestive of septicaemia, pneumonia or meningitis along with isolation of pathogen from blood or CSF or urine. All patients were managed as per unit protocol including appropriate fluid resuscitation, use of inotropes/vasopressors, antibiotics and blood component transfusion.
Data Aanalysis
After collection data was entered into a personal computer and was edited, analyzed and plotted in graphs and tables. Statistical Package for Social Sciences (SPSS) version 21 was used for data analysis. Quantitative data was expressed as mean ± SD and categorical data was presented as proportion. All quantitative variables (between the groups of survivors and non-survivors) were compared by unpaired t-test; categorical variables were compared by Chi-square test. P-value < 0.05 was considered as significant.
Result
108 preterm neonates below 34 weeks were eligible for this study. Four newborns were excluded. 104 newborns were enrolled in this study. Then among 104 preterm neonates 52 were randomized to colostrum group and 52 were randomized to placebo group. All the neonates randomized to colostrum completed the study. Among the placebo group 5 patients were died, parents of 7 patients left against medical advice, finally 40 patients completed the study (Fig. 1).
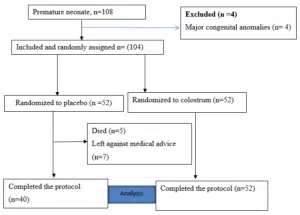
Figure 1: CONSORT flow diagram for study.
General characteristics of mothers and newborns are shown in Table 1 and 2. Baseline characteristics comparable between two groups. Most of the preterm babies gestational age was >28 weeks both in colostrum (94%) and placebo group (87.5%). Birth weight was mostly >1000 gram in both the groups, that is 92% in intervention group and 82.5% in placebo group. Most of the babies were AGA in both the groups. In colostrum group 11.5% was SGA and in placebo group 25% was SGA. Gender distribution reflected slight female predominance 58.3%. Most of the infants were born by LUCS that was 84%. Comparison of the clinical outcome between the intervention and control groups is shown in Table 3.
Our study showed significant reduction in the incidence of LONS 55.7% vs. 85% (p = 0.003); probable sepsis 46.1% vs. 70% (p = 0.033), proven sepsis 36.5% vs. 57.5%( p = 0.058).Among the secondary outcome there was significant reduction of DIC 23% vs. 55% ( p = 0.002),No statistical differences were found on the incidence of shock, Intraventricular hemorrhage, ventilator-associated pneumonia, BPD,ROP needed laser, AKI and duration of NICU were comparable between intervention and placebo groups.
Table 4 showing the comparison of treatment outcome between OAC and control group. The use of mechanical ventilators 21.1% vs. 55% (p = 0.001) and no of inotropes 1.18±0.395vs 1.61±0.497 (p = 0.002), duration of inotropes 19.77±14.249 vs. 36.57±17.502 (p = 0.002) was statistically reduced in OAC group. There were no statistical differences on use of CPAP, fluid boluses and duration of MV between the two groups. A comparison of the serum IgA level at 1st and 7th day between the OAC and control groups is shown in Table 5. There was no statistically significant difference in serum IgA level at 1st and 7th day between intervention and placebo groups.
Characteristics | Colostrum group(n=52) | Placebo group(n=40) | P -Value |
Maternal age | |||
<20 yrs | 4(7.6%) | 0 | 0.063 |
20-30 yrs | 40(76.9%) | 29(72.5%) | |
31-39yrs | 8(15.3%) | 8(20%) | |
>40yrs | 0 | 3 | |
Maternal education | |||
Primary level | 3(5.7%) | 2(5%) | 0.985 |
Secondary level | 21(40.3%) | 16(40%) | |
Higher secondary and above | 28(53.8%) | 22(55%) | |
Parity | |||
Primipara | 24(46.1%) | 11(27.5%) | 0.068 |
Multipara | 28(53.8%) | 29(72.5%) | |
No of antenatal visits | |||
<4 | 3(5.7%) | 5(12.5%) | 0.26 |
>4 | 49(94.2%) | 34(85%) | |
Maternal DM | 7(13.4%) | 5(12.5%) | 0.892 |
Maternal HTN | 24(46.1%) | 17(42.5%) | 0.727 |
Antenatal corticosteroid | |||
None | 1(1.9%) | 2(5%) | 0.681 |
Incomplete dose | 21(40.3%) | 20(50%) | |
Complete dose | 30(57.6%) | 18(45%) | |
PROM>18 hrs | 12(23.07%) | 13(32.5%) | 0.314 |
Antenatal antibiotics | 12(23.07%) | 13(32.5%) | 0.314 |
Table 1: Baseline characteristics of maternal factors (N=92).
Characteristics | Colostrum | Placebo | Value |
group(n=52) | group(n=40) | ||
GA (weeks), n(%) | |||
<28wks | 3(5.7%) | 5(12.5%) | 0.288 |
>28wks | 49(94%) | 35(87.5%) | |
Birth weight n(%), | |||
<1000 grams | 6(8%) | 7(17.5%) | 0.548 |
>1000 grams | 46 (92%) | 33(82.5%) | |
Fetal growth, n(%) | |||
SGA | 6(11.5%) | 10(25%) | |
AGA | 46(88.4%) | 29(72.5%) | 0.113 |
LGA | 0 | 1(2.5%) | |
Sex, n(%) | |||
Male | 31(59.6%) | 19(47.5%) | 0.304 |
Female | 20(38.4%) | 21(52.5%) | |
Mode of delivery, n(%) | |||
LUCS | 47 (90.3%) | 31(77.5%) | 0.94 |
NVD | 4 (9.7%) | 9(22.5%) | |
APGAR score at 1st min, n(%) | |||
>7 | 49(94.2%) | 37(92.5%) | 0.739 |
6-Apr | 3(5.7%) | 3(7.5%) | |
APGAR score at 5th min n(%). | |||
>7 | 52 (100%) | 40(100%) | |
6-Apr | 0 | 0 |
Table 2: Baseline characteristics of neonates (N=92).
Characteristics | Colostrum group (n=52) | Placebo group (n=40) | P-Value |
Clinical sepsis, n(%) | 29(55.7%) | 34(85%) | 0.003 |
Probable sepsis, n(%) | 24(46.1%) | 28(70%) | 0.033 |
Culture positive,n(%) | 19(36.5%) | 23(57.5) | 0.058 |
Ventilator associated pneumonia, n(%) | 4(7.7%) | 10(25%) | 0.022 |
BPD, n(%) | 0 | 2(5%) | 0.103 |
IVH, n(%) | 23(44.2%) | 18(45%) | 0.941 |
ROP needed Laser. n(%) | 10(19.2%) | 15(37.5%) | 0.51 |
Shock, n(%) | 22(42.3%) | 27(67.5%) | 0.016 |
AKI, n(%) | 11(21.1%) | 18(45%) | 0.015 |
DIC, n (%) | 12(23%) | 22(55%) | 0.002 |
Duration of NICU (d), mean±SD | 14.33±5.067 | 16.30±7.240 | 0.128 |
Survived n (%), | 47 | 30 | 0.048 |
Table 3: Clinical outcomes between the colostrum group and placebo group at the time of discharge (N=92).
Treatment modalities | Colostrum | Placebo | P-value |
group(N=52) | group (N=40) | ||
Fluid bolus for shock, n(%) | |||
One | 19(36.5%) | 25(62.5%) | 0.752 |
>one | 3(5.7%) | 3(7.5%) | |
Mechanical ventilator, n(%) | 11(21.1%) | 22(55%) | 0.001 |
Duration of MV(hrs) mean±SD | 5±1.732 | 14.91±13.291 | 0.02 |
CPAP, n(%) | 20(38.4%) | 22(55%) | 0.504 |
Inotrope use(number) mean±SD | 1.18±0.395 | 1.61±0.497 | 0.002 |
Inotrope use duration(hrs) mean±SD | 19.77±14.249 | 36.57±17.502 | 0.001 |
Qualitative data are presented as the number and percentage, Statistical test: Chi-square test was used for categorical data, p < 0.05 were considered as significant. ns- not significant. | |||
Table 4: Comparison of treatment modalities between colostrum and placebo group (N=92).
Characteristics | Colostrum | Placebo | P-value |
group(n=52) | group(n=40) | ||
Serum IgA 1st day | 0.2884±0.12536 | 0.2683±0.5460 | 0.346 |
Serum IgA 7th day | 3.8317±17.102 | 0.2997±0.09303 | 0.195 |
mean±SD |
Table 5: Comparison of serum IgA level between colostrum and placebo group(N=92).
Discussion
Late Onset Neonatal Sepsis (LONS) is still one of the devastating diseases among preterm infants, with significant mortality rates despite advancement of treatment. This single-center, RCT showed a lower incidence of late-onset sepsis and mortality rate in preterm infants with GA ≤ 34 weeks who received colostrum within 24 hrs of life. In addition, the incidence of DIC was lower in the Oropharyngeal Administration of Colostrum (OAC) group. The need for mechanical ventilator, number and duration of inotrope was also decreased. Statistically significant difference was not seen in serum IgA level between the two groups. Colostrum could be applied in buccal mucosa for 5 days after birth or longer, even extending until the baby could receive partial oral feed or reach the corrected gestational age at 32 weeks., In our study preterm infants got benefits in terms of mechanical ventilator use, inotrope use and its duration by oropharyngeal application of colostrum. In the published literature there is variations in the procedure of Oropharyngeal administration of colostrum, including variation in the dosage of colostrum (ranging from 0.1 ml to 0.4 ml, even to 1.0 ml), the duration of each administration (“drop into the oral mucosa” or apply for less than 5 sec), the frequency of treatments for each day (every 2 to 6 h), the duration of the treatment (ranging from 2 to 7 days, or on an as-needed basis, the type of applicator (syringe or swab), and the type of breast milk (fresh or frozen) [9-12]. There is inactivation of some immune protective factors with this approach resulting in decreased levels of this substances [13]. Contamination might also occur, as some studies have shown pathogenic organisms in mother milk samples [14-16]. In our study, 0.2 ml of fresh colostrum was administered in buccal mucosa (0.1 ml in each side of buccal mucosa for 10 second) every 3 hrs for 72 hrs. There were no adverse events, including oral mucosal damage, apnea, bradycardia, tachycardia or desaturation in our study. So, oropharyngeal administration of colostrum is a safe procedure in the NICU for preterm infants. Late onset neonatal sepsis is triggered and influenced by multiple factors such as the status of preterm infants, the therapy received and the medical condition, which are all significant [17]. Colonization of the preterm gut by pathogenic organism appears to be a primary step in the pathogenesis of LONS [18-22]. A pathogenic organism promotes injury to the mucosal barrier and facilitates bacterial translocation from the gut into the bloodstream [23]. Biofactors of milk protect against LONS, by means of it’s antimicrobial, anti-inflammatory and immunomodulatory functions. It also inhibits pathogen adhesion to the gastrointestinal mucosa, enhance gastrointestinal microbiota, maintain the integrity of the intestinal barrier and repair areas of injury, promote intestinal maturation and motility, and provide antioxidant protection [24-27]. The incidence of late-onset clinical sepsis was potentially lower in our study among preterm infants with GA ≤ 34 weeks who received buccal colostrum within 24 hrs of life 55.7% vs. 85%. The risk of developing LONS in the colostrum group was 22% lower in intervention group than in the control group. These results are consistent with those of a previous study by Xia Ou Yang and his team. Their findings were LONS reduced from 13.6 to 4.7% [28]. It also reduces culture proven sepsis, thereby reducing various complications of sepsis such as DIC and mortality rate. Our study results are in-line with the evidences that suggests oropharyngeal colostrum care is safe in VLBW infants.
Limitations
Single centre study.
Conclusion
This study concluded that administration of colostrum administration by oropharyngeal route reduces the incidence of late-onset neonatal sepsis, DIC, use of MV and use of inotropes, duration of inotropes in preterm infant.
Acknowledgments
We are thankful to Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka for providing all types of logistic supports and the facilities for the conduction of this study. This work was supported by the department of neonatology, BSMMU.
Conflict of Interest
The authors have no conflict of interest to declare.
Authors Contributions
Md. Abdul Mannan conceptualized the study, supervised data entry and analyzed data, drafted the first manuscript, edited and finalized the manuscript. Md. Nazmus Sihan and Shazia Afreen have assisted in sample collection, day to day follow up, data entry, subsequent analysis and gave feedback to draft of manuscript. All authors read and approved the final manuscript.
Consent
As per international standard, parental written consent has been collected and preserved by the author(s).
Ethical Approval
As per international standard or university standard written ethical approval has been collected and preserved by the author(s).
Competing Interests: Authors have declared that no competing interests exist.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
- Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008;371(9606):75‐84.
- Slattery MM, Morrison JJ. Preterm delivery. Lancet. 2002; 360(9344):1489‐97.
- Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late‐onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110(2):285‐91.
- Stoll BJ, Hansen NI, Adams‐Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental and growth impairment among extremely low‐birth‐weight infants with neonatal infection. JAMA. 2004;292(19):2357‐65.
- Giannì ML, Sannino P, Bezze E, Plevani L, di Cugno N, Roggero P, et al. Effect of co-morbidities on the development of oral feeding ability in pre-term infants: a retrospective study. Sci Rep. 2015;5(1):16603.
- Rodriguez NA, Meier PP, Groer MW, Zeller JM. Oropharyngeal administration of colostrum to extremely low birth weight infants: theoretical perspectives. J Perinatol. 2009;29(1):1-7
- Neu J, Walker WAN. Engl J Med. 2011 Jan 20; 364(3):255-64.
- World Health Organization, march of dimes, the partnership for maternal, newborn and child health, save the children. Born too soon: the global action report on preterm birth.
- Tao J, Mao J, Yang J, Su Y. Effects of oropharyngeal administration of colostrum on the incidence of necrotizing enterocolitis, late-onset sepsis, and death in preterm infants: a meta-analysis of RCTs. Eur J Clin Nutr. 2020;74(8):1122-31.
- Garg BD, Balasubramanian H, Kabra NS, Bansal A. Effect of oropharyngeal colostrum therapy in the prevention of necrotising enterocolitis among very low birthweight neonates: a meta-analysis of randomized controlled trials. J Hum Nutr Diet. 2018;31(5):612-24.
- Giannì ML, Sannino P, Bezze E, Plevani L, di Cugno N, Roggero P, et al. Effect of co-morbidities on the development of oral feeding ability in preterm infants: a retrospective study. Sci Rep. 2015;5(1):16603.
- Landers S, Updegrove K. Bacteriological screening of donor human milk before and after Holder pasteurization. Breastfeed Med. 2010;5:117-21.
- Schanler RJ, Fraley JK, Lau C, Hurst NM, Horvath L, Rossmann SN. Breastmilk cultures and infection in extremely premature infants. J Perinatol. 2011;31:335-8.
- Zhu XL, Tang XG, Qu F, Zheng Y, Zhang WH, Diao YQ. Bifidobacterium may benefit the prevention of necrotizing enterocolitis in preterm infants: a systematic review and meta-analysis. Int J Surg. 2019;61:17-25.
- Sharma D, Kaur A, Farahbakhsh N, Agarwal S. Role of oropharyngeal administration of colostrum in very-low-birth-weight infants for reducing necrotizing enterocolitis: a randomized controlled trial. Am J Perinatol. 2020;37(7):716-21.
- Martín-Álvarez E, Diaz-Castro J, Peña-Caballero M, Serrano-López L, Moreno-Fernández J, Sánchez-Martínez B, et al. Oropharyngeal colostrum positively modulates the inflammatory response in preterm neonates. Nutrients. 2020;12(2):413.
- Rost BL, Caplan MS. Necrotizing enterocolitis: pathophysiology, platelet-activating factor, and probiotics. Semin Pediatr Surg. 2013;22:88-93.
- Bisquera JA, Cooper TR, Berseth CL. Impact of necrotizing enterocolitis on length of stay and hospital charges in very low birth weight infants. Pediatrics 2002;109(3):423‐8.
- Claud EC. Probiotics and neonatal necrotizing enterocolitis. Anaerobe. 2011;17(4):180-5.
- Carl MA, Ndao IM, Springman AC, Manning SD, Johnson JR, Johnston BD, et al. Sepsis from the gut: the enteric habitat of bacteria that cause late-onset neonatal bloodstream infections. Clin Infect Dis. 2014;58:1211-8.
- Madan JC, Salari RC, Saxena D, Davidson L, O’Toole GA, Moore JH, et al. Gut microbial colonization in premature neonates predict neonatal sepsis. Arch Dis Child Fetal Neonatal Ed. 2012;97:F456-62.
- Meier PP, Bode L. Health, nutrition, and cost outcomes of human milk feedings for very low birthweight infants. Adv Nutr. 2013;17:180-5.
- Meier PP, Bode L. Health, nutrition, and cost outcomes of human milk feedings for very low birthweight infants. Adv Nutr. 2013;4:670-1.
- Kiu B, Newburg DA. Human milk glycoproteins protect infants against human pathogens. Breastfeed Med. 2013;8:354-62.
- Rodríguez NA, Miracle DJ, Meier PP. Sharing the science on human milk feedings with mothers of very low birth weight infants. JOGNN. 2005;34:109-19.
- Nasuf A, Ojha S, Dorling J. Oropharyngeal colostrum in preventing mortality and morbidity in preterm infants. Cochrane Database Syst Rev. 2018;9:CD011921.
- Tao J, Mao J, Yang J, Su Y. Effects of oropharyngeal administration of colostrum on the incidence of necrotizing enterocolitis, late-onset sepsis, and death in preterm infants: a meta-analysis of RCTs. Eur J Clin Nutr. 2020;74(8):1122-31.
- Rodriguez NA, Vento M, Claud EC, Wang CE, Caplan MS. Oropharyngeal administration of mother’s colostrum, health outcomes of premature infants: study protocol for a randomized controlled trial. Trials. 2015;16(1):453.
This work is licensed under a Creative Commons Attribution 2.0 International License.


