Lukinga Witanene Jean Paul1*, Maloba1, Kisaka3, Kasamba3, Mukalayi2, Ben Monga2, Bidilukinu3, Kashind3, Tambwe1, Shombo2, Odile2, Kyundu2, Ngalamulume2, Mutekwa2, Kyabu2, Chilundika2, Chenge1
1Ophtalmology, Senior Assistant University, Clinics of Lubumbashi Specialty, Department Ophthalmology Service, Congo
2Public Health, Senior Assistant University, Clinics of Lubumbashi Specialty, Congo
3Biology, Senior Assistant University, Clinics of Lubumbashi Specialty, Congo
*Correspondence author: Lukinga Witanene Jean Paul, Senior Assistant University, Clinics of Lubumbashi Specialty, Department Ophthalmology Service, Congo; Email: jpwitha@gmai.com
Published Date: 26-03-2024
Copyright© 2024 by Paul LWJ, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Onchocerciasis is the second leading cause of infectious blindness. This condition is serious because of its ocular complications. The sickness is caused through a Nematode specifique of I man Ochocerca Volvulus the transmission se made through a vecteur the Simulie (Mouches blacks circulant autours of the waters at current fast). We have 5 Syndroms: Cutane, Nodulaire, Oculaire, Lymphatique and Neurologique. These complications eyes him at valu the name of cecite of riviere through OMS in 1972. Our objective was to determine the epidemiological profile of onchocerciasis in the Sambwa health area.
Materials and method: We conducted a prospective cross-sectional descriptive study over a period of 5 months (01/01 to 01/05/2023). We included patients whose skin biopsy was positive for onchocerciasis, aged 10 to 90 years old and having lived more than 10 years in Sambwa. The significance threshold was 0.05%. Excel, Word and IBM SPSS 23 software were used for data entry and analysis. One hundred people were examined, 38 of whom were retained.
Results: The frequency of onchocerciasis was 38%, men predominated (57.9%, sex ratio 1.4). The average age was 64.37±11.63 years. Farmers represented 68.4%. Most patients had a stay in Sambwa of 10 to 29 years (42.2%). Ocular syndromes represented 57.6% of cases, of which bilateral cataract (31.6%) predominated, there was an association between age and ocular syndromes (p=0.00011). Blindness represented 31.6% of cases in the right eye while in the left eye mild impairment represented 26.3% of cases. Tonometry between 15.9 and 20.6 mmHg was 81.6% on the right and 76.3% on the left. In most cases the fundus was inaccessible (26.3% on the right and 21.1% on the left). In 47.4% of cases there was a refractive error.
Conclusion: Considering our results, onchocerciasis is a relatively common condition, the Sambwa health area is a Hypoendemic area.
Keywords: Onchocerciasis; Blindness; Sambwa
Introduction
Onchocerciasis is a parasitosis caused by a nematode specific to humans, Onchocerca volvulus, which is found in Africa, the Middle East, South America and Central America [1]. It is the second leading cause of infectious blindness in the world after trachoma. It is transmitted by the female blackfly in places close to fast-moving water. This condition is serious because of its ocular complications which have earned it the name river blindness [2]. The disease manifests itself through particularly disabling skin damage and eye problems which can lead to blindness, depriving patients of their ability to work in the prime of life. Deprived of their most productive population, the villages of the rich fertile valleys were the first to suffer the socio-economic repercussions of the parasitosis. To escape this scourge, people abandoned fertile lands in favor of forest areas that were less infested but barely exploitable. In the 1970s, millions of fertile hectares were deserted [3].
The World Health Organization (WHO) estimates that 120 million individuals are exposed to onchocerciasis and approximately 18 million people are infected, more than 99% of whom live in intertropical Africa, among whom 350,000 are blind [4]. The disease is endemic in 31 countries in sub-Saharan Africa, three countries in Latin America and Yemen. The WHO verified the elimination of parasite transmission in Colombia, Ecuador, Mexico and Guatemala in 2013, 2014, 2015, 2016 respectively and declared these four countries free of the disease (Fig. 1,2) [5].
Rural communities that live near turbulent waterways are the most exposed: this is where blackflies, vectors of the disease, reproduce [3].

Figure 1: Zone de santé de Kafubu.
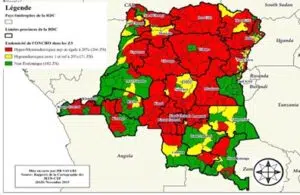
Figure 2: Cartographie épidémiologique /RDC /OMS: 2015.
Material and Methods
Type of Study, Subjects and Study Area
This is a cross-sectional descriptive study with prospective data collection which lasted from January 1 to May 1, 2023, a period of 5 months.
Our study concerned all people aged 10 to 90 living in the Sambwa health area. The cut theoretical d sample tire sure the formule of Cochran n = z² x p (1-p) / m² (1 ,96)²X 0,48 ( 1- 0,48)/ (0,05)²꓿ 3,8416 X 0,48 ꓿ 1,843968 (1- 0,48) ꓿ 0,52. 1,843968 X 0,52 ꓿ 0,95886336/0,0025 ꓿ 383.
We opted for non-probability convenience sampling following the inclusion and non-inclusion criteria. 100 people were examined during the study period.
Inclusion Criteria
Suffering from onchocerciasis; Undergo a clinical examination and additional investigations having confirmed the diagnosis of onchocerciasis; Freely agree to participate in the study; Be between 10 and 90 years old; Have lived in the Sambwa health area for more than 10 years.
Non-Inclusion Criteria
Patients Not Suffering from Onchocerciasis
Those who have not carried out additional investigations to confirm the diagnosis of onchocerciasis; Those with onchocerciasis but who refused to participate in the study.
Research Team and Meetings with Patients
A team of seven investigators (a Senior Doctor in ophthalmology, A Biological Doctor, A General Practitioner, A laboratory technician, Two Sensitizers and A head of the local onchocerciasis branch) with well-defined tasks was responsible for collecting the data to based on a standardized survey form [3-10].
Method and Diagnosis
Complete Clinical Examination
Questioning: Identity, lifestyle, stay in Sambwa, duration of ivermectin treatment, profession, height, telephone number as well as the patient’s complaints [11-22].
Inspection: looking for skin lesions.
Palpation: to assess the number of nodules and their location.
Results and Discussion
38 cases of onchocerciasis out of 100 people examined: 38% of cases (Sambwa hypoendemic zone) Chenge B. 47.59%, Kapoli W. in the city of Inga: 58% [3-12].
Sociodemographic Characteristics
Age
Extremes: 43 years to 85 years, average: 64.37±11.63 years. Kapoli W: 39.12 years, IDEM Chenge B and Maertens K.: Decline in disease at extreme ages (Fig. 3,4).

Figure 3: Prevalence of onchocerciasis in the Sambwa health area.

Figure 4: Distribution of patients according to age groups.
Gender
It appears from the figure below that the male gender predominated with 57.9% or a sex ratio of 1.38.
Sex ratio of 1.38 (Fig. 5).

Figure 5: Distribution of patients by gender.
Masc Predominance: Chenge B; Kapoli
Size
The average height of our patients was 165.45 ± 5.49 cm, most had a height ≥ 159 cm (Fig. 6) [13].

Figure 6: Distribution of patients according to Talle.
Profession (Table 1)
|
Profession |
Effective |
Percentage |
|
Farmer |
26 |
68,4 |
|
Fisherman |
5 |
13,2 |
|
Others |
7 |
18,4 |
|
Total |
38 |
100,0 |
|
Others: priest, teachers, carpenter, shoemaker; Farmers predominated with 68.4% of cases |
||
Table 1: Distribution of patients according to profession.
Stay
It appears from this table that patients aged 10 to 19 years, 20 to 29 years and 60 to 69 years were in the majority with 21.1% of cases for each group. The average length of stay was 36.26 ± 19.71 years (Table 2,3) [24-50].
|
Stay Sambwa |
Effective |
Percentage |
|
10 to 19 years old |
8 |
21,1 |
|
20 to 29 years old |
8 |
21,1 |
|
30 to 39 years old |
4 |
10,5 |
|
40 to 49 years old |
7 |
18,4 |
|
50 to 59 years old |
3 |
7,9 |
|
60 to 69 years old |
8 |
21,1 |
|
Total |
38 |
100,0 |
Table 2: Distribution of patients according to stay in Sambwa.
|
C |
Effective |
% |
Littérature |
Littérature |
|
|
Profession |
Agriculteurs Pécheurs Autres |
26 5 7 |
68,4 13,2 18,4 |
Chenge B : 52,8% agricult et pecheur Kapoli W: 44, 85 % pêcheurs et 20, agriculteurs. |
Chenge B : 52,8% agricult et pecheur Kapoli W: 44, 85 % pêcheurs et 20, 75% agriculteurs. |
|
Séjour à Sambwa |
Moy: 36,26 ± 19,71 ans. |
||||
|
Prise Ivermectine |
1 à 3 ans |
23 |
60,5 |
Table 3: Distribution of patients according to profession in Sambwa.
Types of Ophthalmological Lesions
Eye Syndromes (Fig. 7, Table 4)

Figure 7: Above image tells us that ocular manifestations were present in 22 patients or 57.9% of cases.
|
Paramètres |
Effectif |
% |
Littérature |
|
Cataracte |
12 |
31,6 |
Chenge B: 67%; Kapoli W: 67,2%. Maertens K: 16%; Kanke N: 21%. |
|
Conjonctivite |
4 |
10,5 |
|
|
Kératite sclérosante |
4 |
10,5 |
|
|
Choriorétinite |
4 |
10,5 |
|
|
KPS |
2 |
5,3 |
|
|
Uvéite |
2 |
5,3 |
|
|
Glaucome |
2 |
5,3 |
Table 4: Distribution of patients according to disease in Sambwa.
Age and Eye Syndrome Bivariate Analysis (Table 5)
|
Age |
Syndrome oculaire |
|||
|
Non |
% |
Oui |
% |
|
|
≤64,37 |
13 |
81,3 |
4 |
18,2 |
|
>64,37 |
3 |
18,8 |
18 |
81,8 |
|
Total |
16 |
100,0 |
22 |
100,0 |
|
(p=0.00011; X²=14.9). Small p being ≤ at our significance level of 0.05, the difference is statistically significant. That is, there is an affinity between age and ocular syndrome |
||||
Table 5: eye syndrome patient details.
Profession and Eye Syndrome (Table 6)
|
Profession |
Syndrome Oculaire |
|||
|
Non |
% |
Oui |
% |
|
|
Agriculteur |
11 |
68,8 |
15 |
68,2 |
|
Pécheur |
1 |
6,3 |
4 |
18,2 |
|
Autres |
4 |
25,0 |
3 |
13,6 |
|
Total |
16 |
100,0 |
22 |
100,0 |
|
(p=0.37; X²=0.796). Small P being ≥ our significance level of 0.05, the difference is not statistically significant |
||||
Table 6: Distribution of patients with eye syndrome as per profession in Sambwa.
Conclusion
Prevalence: 38% (hypo-endemic zone) This result can be explained by the effectiveness of the fight devoted to CDTI/MMA for 11 years already. This result also illustrates the participation of the different actors (Government, WHO, APOC, PNLO, MTN) including the community itself in the CDTI/MMA process in this Sambwa home. These results allow us to talk about the control and not the elimination of Onchocerciasis in the Sambwa focus. Ages 70 to 79 years, male, farmers, Stay in Sambwa Average: 36.26 years. Ocular syndromes 57.9%, cataract +++, also: Conjunctivitis, Sclerosing keratitis and Ridley’s chorioretinitis. Visual acuity, tonometry and fundus examination were within normal range in the majority of patients. refractive errors were less frequent.
Conflict of Interests
The authors have no conflict of interest to declare.
References
Review Article
Received Date: 26-02-2024
Accepted Date: 18-03-2024
Published Date: 26-03-2024
Copyright© 2024 by Paul LWJ, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Paul LWJ, et al. Epidemio-Clinical Profile of Onchocerciasis in Sambwa in the Democratic Republic of Congo. J Ophthalmol Adv Res. 2024;5(1):1-9.

Figure 1: Zone de santé de Kafubu.

Figure 2: Cartographie épidémiologique /RDC /OMS: 2015.

Figure 3: Prevalence of onchocerciasis in the Sambwa health area.

Figure 4: Distribution of patients according to age groups.

Figure 5: Distribution of patients by gender.

Figure 6: Distribution of patients according to Talle.

Figure 7: Above image tells us that ocular manifestations were present in 22 patients or 57.9% of cases.
Profession | Effective | Percentage |
Farmer | 26 | 68,4 |
Fisherman | 5 | 13,2 |
Others | 7 | 18,4 |
Total | 38 | 100,0 |
Others: priest, teachers, carpenter, shoemaker; Farmers predominated with 68.4% of cases | ||
Table 1: Distribution of patients according to profession.
Stay Sambwa | Effective | Percentage |
10 to 19 years old | 8 | 21,1 |
20 to 29 years old | 8 | 21,1 |
30 to 39 years old | 4 | 10,5 |
40 to 49 years old | 7 | 18,4 |
50 to 59 years old | 3 | 7,9 |
60 to 69 years old | 8 | 21,1 |
Total | 38 | 100,0 |
Table 2: Distribution of patients according to stay in Sambwa.
C | Effective | % | Littérature | Littérature | |
Profession | Agriculteurs Pécheurs Autres | 26 5 7 | 68,4 13,2 18,4 | Chenge B : 52,8% agricult et pecheur Kapoli W: 44, 85 % pêcheurs et 20, agriculteurs. | Chenge B : 52,8% agricult et pecheur Kapoli W: 44, 85 % pêcheurs et 20, 75% agriculteurs. |
Séjour à Sambwa | Moy: 36,26 ± 19,71 ans. | ||||
Prise Ivermectine | 1 à 3 ans | 23 | 60,5 |
Table 3: Distribution of patients according to profession in Sambwa.
Paramètres | Effectif | % | Littérature |
Cataracte | 12 | 31,6 | Chenge B: 67%; Kapoli W: 67,2%. Maertens K: 16%; Kanke N: 21%. |
Conjonctivite | 4 | 10,5 | |
Kératite sclérosante | 4 | 10,5 | |
Choriorétinite | 4 | 10,5 | |
KPS | 2 | 5,3 | |
Uvéite | 2 | 5,3 | |
Glaucome | 2 | 5,3 |
Table 4: Distribution of patients according to disease in Sambwa.
Age | Syndrome oculaire | |||
Non | % | Oui | % | |
≤64,37 | 13 | 81,3 | 4 | 18,2 |
>64,37 | 3 | 18,8 | 18 | 81,8 |
Total | 16 | 100,0 | 22 | 100,0 |
(p=0.00011; X²=14.9). Small p being ≤ at our significance level of 0.05, the difference is statistically significant. That is, there is an affinity between age and ocular syndrome | ||||
Table 5: eye syndrome patient details.
Profession | Syndrome Oculaire | |||
Non | % | Oui | % | |
Agriculteur | 11 | 68,8 | 15 | 68,2 |
Pécheur | 1 | 6,3 | 4 | 18,2 |
Autres | 4 | 25,0 | 3 | 13,6 |
Total | 16 | 100,0 | 22 | 100,0 |
(p=0.37; X²=0.796). Small P being ≥ our significance level of 0.05, the difference is not statistically significant | ||||
Table 6: Distribution of patients with eye syndrome as per profession in Sambwa.