Review Article | Vol. 6, Issue 1 | Journal of Clinical Immunology & Microbiology | Open Access |
Molecular Mechanisms of Antibiotic Resistance in Seafood-Associated Salmonella Enterica: A Brief Review
Parmanand Prabhakar1*, Sanath Kumar H2, Pooja Saklani1, Srinu Rathlavath3, Md. Aman Hassan1, Sarvendra Kumar1
1College of Fisheries (Bihar Animal Sciences University), Kishanganj, Bihar, India
2Quality control laboratory, ICAR-Central Institute of Fisheries Education, Mumbai, India
3College of Fisheries Science, Uttar Pradesh Pandit Deen Dayal Upadhyaya Pashu Chikitsa Vigyan Vishwavidyalaya Evam Go-Anusandhan Sansthan (DUVASU), Mathura 281001, India
*Correspondence author: Parmanand Prabhakar, College of Fisheries (Bihar Animal Sciences University), Kishanganj, Bihar, India; Email: [email protected]
Citation: Prabhakar P, et al. Molecular Mechanisms of Antibiotic Resistance in Seafood-Associated Salmonella Enterica: A Brief Review. J Clin Immunol Microbiol. 2025;6(1):1-10.
Copyright© 2025 by Prabhakar P, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 18 March, 2025 | Accepted 13 April, 2025 | Published 20 April, 2025 |
Abstract
The consumption of seafood has risen across the world. The incidence of seafood-associated bacterial infections also rose, with Salmonella sp. being of significant concern. There are various Salmonella serotypes exist; Salmonella enterica serovar Typhimurium and Enteritidis have garnered major attention as seafood-borne pathogens. The disease-causing capacity of Salmonella is attributed to its ability to express a wide assemblage of virulence factors that help the bacterium invade, colonize and survive in seafood environments and in the gastrointestinal tracts of humans. More than this, the emergence of antimicrobial resistance in Salmonella detected from seafood is a significant task for the seafood industry in safeguarding the health of humans worldwide. Implementation of comprehensive surveillance programs, good aquaculture practices, proper handling, processing and adherence to strict food safety regulations and food safety management are needed to minimize the Salmonella contamination in seafood. This study is focused on the antimicrobial resistance in Salmonella involved in different types of seafood.
Keywords: Salmonella; Seafood; Antimicrobial Resistance; Pathogen; Public Health
Introduction
The Gram-negative bacterium Salmonella enterica, belonging to the family Enterobacteriaceae, is one of the leading causes of food-borne gastroenteritis worldwide. Salmonella is a human and animal-associated pathogen and its presence in foods and the environment is due to contamination from these sources. Salmonella infections are manifested as diarrhea, fever, vomiting and abdominal cramps [1,2]. Infection due to Salmonella is an important public health concern across the world, along with an economic burden because of the expenses of disease control and treatment [3-5]. Other manifestations of Salmonella infections include bacteremia, meningitis, urinary tract infections, etc. S. enterica comprises more than 1500 serotypes distributed over diverse sources [6]. Typhoidal strains of Salmonella, namely S. Typhi and S. Paratyphi, are exclusively associated with humans, while all other serovars are widely distributed in animals, birds, reptiles, etc [7]. Food-borne salmonellosis is one of the leading causes of human illness worldwide [8]. Every year, 1.4 million cases of food-borne salmonellosis occur in the US alone [9]. Worldwide, non-typhoidal Salmonella are responsible for 93.8 million food-borne infections and 1, 55, 000 deaths annually [10]. Although infections by non-typhoidal Salmonella are generally self-limiting, they cause considerable morbidity due to their widespread presence in foods of different origins. Approximately 95 % of cases of salmonellosis are associated with consuming contaminated products like meat, eggs, poultry, milk, fresh produce and seafood [11]. Fish and shellfish are not known to harbor Salmonella as their natural biota. Salmonella in seafood is due to the secondary contamination occurring at various stages, from harvest to consumption [12]. Fish in their natural habitat are contaminated by bacterial pathogens due to the discharge of domestic, agricultural wastes and land runoff.
Salmonella can be found in the digestive tracts of birds, reptiles, animals and humans. Common serotypes of Salmonella have been involved with direct or indirect contact with reptiles such as turtles, snakes, lizards and iguanas) [13]. Food and water can be contaminated with Salmonella by coming in contact with the feces of infected people or animals [14]. In addition to being a healthy food with high nutritional value seafood can be associated with high risks, mainly those related to bacterial contamination. Significant epidemiological data is available on the presence of Salmonella in seafood and related illnesses, stressing the need for Salmonella risk management in seafood. The occurrence of Salmonella in aquaculture fish products due to the use of untreated or contaminated water during production and cross-contamination while handling and transportation is a significant public health concern. In aquatic environments, the survival rate of Salmonella is very high and can survive longer than V. cholerae in highly eutrophic river water [15].
Salmonella contamination is a major problem in farmed fish and shellfish. The incidence of salmonellosis in many countries due to the consumption of contaminated seafood, such as uncooked shellfish, is a primary concern of public health agencies [16]. Seafood, particularly shellfish in the United States, accounted for 7.42 % of all food poisoning-related deaths due to Salmonella infections from 1990 to 1998 [11]. In recent decades, the per capita consumption of seafood and aquaculture products has increased significantly [17-19]. With this, potential risks of exposure to foodborne pathogens have also increased.
In recent years, antimicrobial resistance among non-typhoidal Salmonella has been on the rise, presumably due to the use of antimicrobial agents in food animals [20,21]. Most infections with antibiotic-resistant Salmonella are acquired by eating contaminated foods of animal origin [22]. Unregulated doses of antibiotics in fish culture ponds can also significantly contribute to the rise in antibiotic-resistant bacteria in seafood [23]. The presence of antibiotic-resistant bacteria in seafood produced in or exported to developed countries has been reported by many authors [24,25]. This is especially important in East and Southeast Asia, where most aquaculture production and consumption occurs [26].
Antibiotic Resistance
Antimicrobial resistance is a major public health issue in all over the world [27,28]. Bacteria exhibit antibiotic-resistant properties owing to three basic mechanisms such as (i) modification of the antibiotic by reducing antibiotic absorption or increasing efflux of the antibiotic drugs by using their enzymes, (ii) alteration of the target site of the antibiotics and (iii) acquisition of the capacity to alter or break the antibiotic [29]. Various lines of corroboration reveal that the application of antimicrobial agents in food animals contributes to the emergence and circulation of antimicrobial resistance in food-borne Salmonella [30]. In the current scenario, antimicrobial resistance is a serious issue that impedes the treatment of salmonellosis [31,32]. The prevalence of antimicrobial-resistant bacteria worldwide occurs due to the epidemic spread of a specific bacterial isolate and the genetic material exchange from one microbe to another. The emergence of Multidrug-Resistant (MDR) Salmonella serovars limits therapeutic options in both humans and animals [33]. Treatment of gastrointestinal illness posed by NTS does not recommend antimicrobial treatment in healthy humans as the infection often is self-limiting. Individuals suffering from severe illness, immune suppression or bacteremia are given antimicrobial therapy [7]. Application of first-line antimicrobial drugs should include ampicillin, chloramphenicol or trimethoprim-sulfamethoxazole [7,34].
History of Antimicrobial Resistance in Salmonella
The antibiotic chloramphenicol, which was discovered in 1948, was very effective as a drug for typhoid fever and was used on a large scale. After two years, chloramphenicol-resistant S. Typhi was reported from England [35], probably due to its indiscriminate application. However, it was not a major problem till 1972. Salmonellosis outbreaks were continuously being reported in Mexico (1972), India (1972), Vietnam (1973) and Korea (1977). Ampicillin was also reported to be ineffective against this strain. Till 1975, co-trimoxazole remained an effective alternative drug until resistance to it was reported in France. By the end of 1980s, strains of S. Typhi became resistant to all these three antibiotics [36]. Multidrug-Resistant Typhoid Fever (MDRTF) can be defined as typhoid fever due to S. Typhi strains that are resistant to three first-line recommended drugs for treatment such as ampicillin, chloramphenicol and co-trimoxazole [37]. The repeated occurrence of MDRTF in children prompted the use of ciprofloxacin. The following studies showed that ciprofloxacin was safe, effective and less expensive for children. Therefore, fluoroquinolones have started to be used across the world as the drug of choice for the treatment of MDRTF. In 1992, S. Typhi, resistant to fluoroquinolones, was reported in the United Kingdom and other nations, including India. With the resistance development of quinolone (nalidixic acid), third-generation cephalosporins were used, but sporadic reports of resistance to them were also observed [38]. A report by Elhadi (2014) in Saudi Arabia, the isolated Salmonella sp. from seafood were exhibited the highest rate of resistance to antibiotics such as tetracycline (90.71%), ampicillin (70%) and amoxicillin-clavulanic acid (45%) [39].
Plasmid Profiles of Salmonella
Virulence plasmids are a well-defined category of plasmids found in Salmonella, with sizes ranging from 2 to 200 kb [40]. Plasmid-mediated resistance occurs when antimicrobial-resistant genes carried on plasmids are transferred from one prokaryote to another via horizontal gene transfer. Bacteria can transmit plasmids from one cell to another via conjugation, allowing antibiotic-resistant plasmids to spread throughout bacterial cells [41]. The presence of plasmid-borne virulence genes in Salmonella was initially suggested in 1982. However, recent evidence suggests that virulence plasmids have a lesser role in Salmonella pathogenesis than in E. coli, Yersinia spp. and Shigella spp. [42]. Only a few Salmonella serovars, primarily from subspecies I, have been identified to possess virulence plasmids, including S. Paratyphi C, S. Enteritidis, S. Typhimurium, S. Dublin, S. Choleraesuis, S. Gallinarum and S. Pullorum [43]. These plasmids are known as “serovar-specific plasmids,” and their size ranges from 50 to 90 kb; however, not every isolate of a plasmid-bearing serovar carries the virulence plasmid [44 – 46]. Salmonella Typhi Salmonella Paratyphi A, Salmonella Paratyphi B and Salmonella Sendai do not contain virulence plasmids and the SPV region [43,46]. To confer the virulent phenotype, only a 7.8 kb region, SPV (Salmonella plasmid virulence), is necessary and other loci of the plasmid implicated in the synthesis of fimbriae and serum resistance may play a role in different phases of the infection. The spv region of Subspecies I contains five genes known as spvRABCD, which are thought to contribute to colonization and resistance to complement killing by the rck gene [44]. The pef (plasmid encoded fimbriae) locus contains four genes designated as pefBACD and additional ORFs (orf5, orf6, orf7, orf8, orf9 and orf11) whose function cannot be determined from sequence analysis [47]. The known gene rck involved in serum resistance was found between the last two ORFs. Plasmids of Salmonella Enteritidis and Salmonella Typhimurium carry the per gene, which determines the formation of surface filamentous structures [42]. Baumler, et al., demonstrated that PEF mediates adherence to the small intestine of mice, when used pefC insertion mutants of Salmonella Typhimurium. The role of resistance in Salmonella to bacteriolytic activity of normal serum was found to be mediated by the long-chain Lipopolysaccharide (LPS) of Salmonella. Three virulence plasmid genes, traT, rck and rsk, have been suggested to be involved in serum resistance [42].
Transposons: Other than transposition, transposons in bacteria may carry additional genes for functions like resistance to antibiotics. Transposons in bacteria can jump to plasmid DNA from chromosomal DNA and back, causing the transfer and permanent addition of genes, such as those encoding antibiotic resistance [49]. This way, a resistant gene can be directly incorporated into host chromosomal DNA and need no dependence on plasmid transfer for spread [41]. It is also observed that integrons have been associated with the widely distributed transposon Tn21. The Tn21 transposon encodes genes and sites required for transposition (including tnpA, tnpR, tnpM, res and inverted repeats) and integrons are located in the left arm, adjacent to the tnpM gene [50]. The aadA1 gene cassette is found to confer resistance to streptomycin and spectinomycin in Tn21-associated integrons [50]. Streptomycin resistance genes such as strA-strB and tet(A) resistance gene are also found encoded in transposon Tn5393. They are frequently located on plasmids of multidrug-resistant S. enterica strains of different serotypes [51].
Integrons: Integrons form an essential ‘building block’ of many transposons and allow the rapid formation and expression of new combinations of genes in response to selection pressures [52]. The prevalence of integrons in multidrug- resistant serotypes of Salmonella is widespread and documented in several studies [53]. Khan, et al., reported the presence of class 1 integrons in S. Bareilly and S. Oslo. Recchia and Hall reported about 60-100 gene cassettes located on integrons responsible for bacterial resistance to a broad spectrum of antimicrobial agents [54,55]. Gene cassettes present in resistance integrons encode resistance to antibiotics, while gene cassettes within super integrons encode a variety of functions. There are four classes of integrons, of which two classes are found in Salmonella [56]. Class 1 integrons called In2 are found associated with transposon Tn21, a member of the Tn3 family of transposable elements and In2 and Tn21 are found widely distributed in Gram negative bacteria [51]. Class 2 integrons are found associated with the Tn7 family of transposons [57].
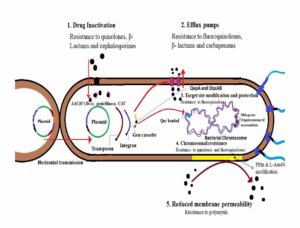
Figure 1: Transmission and antibiotic resistance mechanisms in Salmonella spp. [58-61].
Antibiotic Resistance Mechanisms in Salmonella
In Salmonella enterica, the horizontal transmission of antibiotic-resistance genes located in the plasmid or within the chromosome contributes to the dissemination of antibiotic resistance [62]. Under antibiotic pressure, bacteria that are resistant to one antimicrobial agent quickly evolve and soon develop resistance against other multiple drugs [63]. Bacteria resist antimicrobial activity by: inactivation of the antimicrobials, alteration of the antimicrobial target site, efflux or transport of the antimicrobials and limiting the permeability of the antimicrobial agent (Fig. 1) [59]. Antimicrobial resistant genes acquired by integrons, plasmids or transposons can transfer resistance to other bacterial species or strains. Transposons can transfer antibiotic resistance genes, allowing them to recombine with the chromosome or plasmid. Integrons are composed of the recombination enzyme integrase encoded by the intI gene, a recombination site identified by integrase. Cassettes existing in the integrin are expressed by promoters which are essential gene [64]. These systems efficiently improve the acquisition of external genes such as antibiotic resistance genes in the bacterial genome, primarily through plasmids. Furthermore, conjugation facilitates the transmission of resistance genes existing in plasmids via integron or transposon into the other bacterial species or strains [63].
S. Typhimurium DT104 showing resistance to the trimethoprim is linked to mobile non-conjugative plasmids [65]. S. Typhimurium definitive type (DT) 104 is a multidrug-resistant pathogen that has posed a severe threat to animal husbandry. It was initially discovered in the United Kingdom. It has been associated with animals (monogastric) and ruminants, which are responsible for foodborne outbreaks through meat and meat products. This phage is chromosomally encoded and resistant to more than five drugs, such as ampicillin, chloramphenicol, florfenicol, streptomycin, sulfonamides and tetracyclines. Resistance to fluoroquinolones in non-typhoidal Salmonella is particularly concerning, as fluoroquinolones is the treatment of choice for invasive salmonellosis in adults. The genes that code for gyrase (gyrA and gyrB) and topoisomerase IV target fluoroquinolones in bacterial cells and mutations in these genes cause fluoroquinolone resistance [65,66].
Plasmid-Mediated Quinolone Resistance (PMQR) genes, such as oqxAB and aac(6′)-Ib-cr, are also found in ciprofloxacin-resistant clinical isolates of S. Typhimurium at higher frequencies of 44% and 89%, respectively. The mutation of the PMQR genes, together with the gyrA gene, increases the minimum inhibitory concentration of ciprofloxacin in S. Typhimurium by fourfold. To inhibit fluoroquinolone impact on PMQRs, qnr genes are attached to DNA gyrase and topoisomerase. Fluoroquinolones are ejected into the extracellular space and the PMQR gene, qepA, is closely associated with efflux pumps [67]. Therefore, the combined effect of the mechanism is responsible for the resistance of non-typhoidal Salmonella towards fluoroquinolones [68]. Non-typhoidal Salmonella spp. has developed extended-spectrum resistance to cephalosporins, particularly ceftriaxone, which is a severe concern because these medicines are used to treat invasive non-typhoidal salmonellosis in children. Salmonella develops resistance to β-lactam antibiotics mostly through enzyme hydrolysis [69]. In Salmonella, the first TEM-type β-lactamase, TEM-3, was identified, which displayed the features of ESBL [70-72]. Around 90 types of TEM and 25 types of SHV (sulphydryl variable) β-lactamases are found in the environment [70,73].
Plasmid-mediated ESBLs, such as Cefotaxime (CTX-M), are one of the major concerns since they are often detected in Salmonella spp. and play a role in the hydrolysis of cefotaxime. CTX-M ESBL genes horizontally transfer via conjugation plasmids and transposons, which are primary active processes linked with CTX-M ESBLs acquisition. CTX-M-type β-lactamase expansion differs from that of TEM- and SHV-type β-lactamases, which share similar amino acid changes [71]. However, it has been observed that the serine residue at position 237 in CTX-M enzymes contributes significantly to extended-spectrum antibiotic resistance [74]. In Salmonella, ESBLs genes such as blaTEM-1 and blaSHV-1 confer resistance to third-generation cephalosporins. Genes such as blaCTX-M and blaSHV-5 encoded on transferable plasmids can pose a severe threat to present antibiotic treatment strategies in humans [62].
OXA-type β-lactamases can withstand cephalolecithin and ampicillin. It also has high hydrolytic activity against oxacillin and cloxacillin [75]. Salmonella generates OXA-48 carbapenemase (S. Kentucky) and OXA-1 encoding poultry isolates have been reported [72,76]. Non-Typhoidal Salmonella (NTS) PER-type ESBLs that hydrolyze penicillins and cephalosporins have also been identified [77]. Non-Typhoidal Salmonella frequently produces intrinsic cephalosporinases such as DHA, CMY and ACC-1 enzymes [65,77]. Salmonella serovars contain β-lactamases such SHV-9, CMY-7 and OXA-30, indicating strong cross-resistance among non-typhoidal Salmonella strains [78]. In aminoglycoside antibiotics, the aminoglycoside acetyltransferases modify amino groups. The genes that encode aminoglycoside acetyltransferases are known as aac and they are commonly found in Salmonella genomic islands, integrons and plasmids. Acetyltransferases enzymes provide resistance to important antibiotics viz. kanamycin and gentamicin. The aminoglycoside hydroxyl group of phosphorylating enzymes, such as aminoglycoside phosphotransferases, has been linked to the development of resistance against aminoglycoside antibiotics in Salmonella. Some aminoglycoside phosphotransferases are resistant to neomycin and kanamycin. Among several forms of aminoglycoside adenylyltransferase enzyme coding genes, aadA provides resistance to streptomycin and aadB to gentamicin and tobramycin in Salmonella [79].
Levy, et al., discovered the tetracycline efflux pump (Tet) [80]. Efflux pumps are plasma membrane proteins in bacteria that aid in drug elimination. They are relatively nonselective and may pump a wide range of medicines, including quinolones; these transport proteins are called Multidrug-Resistant (MDR) pumps. The host bacterial cells carrying the plasmid pBR322 were discovered to lower the concentration of tetracycline antibiotic in the cell. The delayed phase of antibiotic efflux benefits the bacteria because it gives them enough time to adapt to the antibiotics and become resistant through mutations or changes in drug targets [81]. Salmonella efflux mechanism mostly involves tet genes, which provide resistance to chlortetracycline, doxycycline, oxytetracycline and tetracycline [82]. However, from clinical or retail meat isolates tet(B), tet(C), tet(D), tet(G) and tet(H) genes have been reported in non-typhoidal Salmonella [79,83]. Tet(A) genes have been found in integrons, plasmids and genomic island 1, while tet(B) genes have been discovered in transferable plasmids. The tet(A) genes have been detected in some Salmonella serovars namely S. Typhimurium, S. Agona, S. Dublin, S. Choleraesuis and S. Heidelberg [79].
The sul gene in Salmonella is responsible for sulfonamide resistance. Common sul genes, such as sul1, sul2 and sul3, are present in major Salmonella serovars such as S. Enteritidis, S. Typhimurium, S. Heidelberg and S. Hadar. Denyer, et al., reported that resistance to sulphonamides is achieved by a plasmid-encoded transport system that actively expels the drug out of the cell [84]. These genes are primarily found in integrons, Salmonella Genomic Islands (SGIs) or transferrable plasmids [79]. The other gene, dhfr, is responsible for expressing a trimethoprim insensitive form of Dihydrofolate Reductase (DHFR). These genes are strongly connected with integrons, Salmonella genomic islands or plasmids [79].
The development of antibiotic resistance in opposition to phenicol antibiotic drugs such as chloramphenicol and florfenicol occurs by two key mechanisms: enzymatic inactivation of antibiotics by chloramphenicol O-acetyltransferase and the efflux pump. Chloramphenicol O-acetyltransferase cannot inactive the florfenicol because the acetyl group of at fluorinated C-3 position in florfenicol is not accepted [85]. O-acetyltransferases genes are often known as cat genes and are frequently associated with plasmids. cat1 and cat2 are the two most common genes found in non-typhoidal Salmonella serovars. The cat genes interact with plasmids, transposons or gene cassettes and other genetic mobile elements [79].
Prevalence of Antibiotic-Resistant Salmonella in seafood
Seafood is one of the most frequently implicated carriers for the spread of antibiotic-resistant bacteria [16,86,87]. The regular use of antimicrobials in food animals has resulted in the development of resistant bacteria in the food chain and excreta of these food animals will pollute the environment with such bacteria, which in turn may be transmitted to humans via water or food. Filter-feeding animals such as oysters and clams can accumulate higher concentrations of bacteria than the surrounding water, which leads to biomagnification of pathogenic bacteria [88]. In the United States, antibiotic-resistant Salmonella (24%) were found in imported seafood identified as, S. Newport, S. Typhimurium var. Copenhagen and S. Lansing. They were resistant to trimethoprim-sulfamethoxazole combination, sulfisoxazole, tetracycline, streptomycin and spectinomycin [87]. Another study found that farm-raised shrimps were more resistant to antibiotics than wild-caught shrimps. Farmed shrimps harbored 9.8 %, 3.6 % and 10.5 % of Salmonella serovar with reduced susceptibility to chloramphenicol, ceftriaxone and tetracycline, respectively, whereas wild-caught shrimps, 2.8%, 1.4% and 1.1 % bacterial isolates showed reduced susceptibility to these antibiotics which was lower than the farm-raised shrimp. From farm-raised shrimp, one Salmonella isolate was resistant to ampicillin, ceftriaxone, gentamicin, streptomycin and trimethoprim [89].
Several investigations found the presence of antibiotic-resistant Salmonella in a variety of seafood such as oysters and fish, fresh fish and fish and shellfish [24,55,90-92]. A study found that two Salmonella strains from serovars Oslo and Bareilly were resistant to trimethoprim/sulfamethoxazole, sulfisoxazole, ampicillin, tetracycline and chloramphenicol antibiotics in the United States between 2000 and 2005 [55]. Two isolates harbored class I integrons, indicating that the resistance genes might easily be transmitted to other harmful bacteria. A study between 2006 and 2012 from Shanghai, China reported 179 isolates of Salmonella were resistant ciprofloxacin. Of these 17 (9.49%) isolates were obtained seafood sources [93]. Another study from India revealed that 59 Salmonella isolates were isolated from seafood comprising 6 different non-typhoidal Salmonella Serovars. Of this, 50% of isolates were shown to multidrug resistant, with the highest resistance to nalidixic acid followed by cotrimoxazole [94]. A recent study reported that all (n=89) serotyped Salmonella recovered from seafood were exposed to antibiotic sensitivity profiling by conventional disc diffusion method. The results of antibiotic sensitivity assay revealed that 12.9 % of the isolates were resistant to more than 6 antibiotics. Resistance to clinically significant antibiotics belonging to cephalosporin and fluoroquinolone groups of antibiotics, although less frequently, is a matter of concern. The study also detected blaCTX-M in 8 isolates resistant to β-lactams, qnrD and qnrS in 4 quinolone resistant isolates and tetB in 2 tetracycline resistant isolates [95]. The emergence of numerous antibiotic-resistant bacteria in seafood is causing increasing worry. Because there are no strict rules prohibiting the overuse and misuse of antibiotics, resistance develops and spreads quickly from the food chain to the environment and to humans, culminating in an antibiotic-induced vicious cycle. The rise of antibiotic-resistant bacteria has already posed a severe threat to human health and it is only growing with the usage of antibiotics. From a seafood safety standpoint, quick action is required to prevent the spread of antibiotic-resistant microorganisms via seafood.
Conclusion
Salmonellosis is a major public health concern worldwide. According to various studies, infection due to Salmonella is not only restricted to poor hygiene and it may not be able to control or eradicate Salmonella contamination in seafood, Fish and shellfish and seafood products by simply controlling indicator organism levels. Moreover, the development of Multi-drug resistant Salmonella Serovars presents a major difficulty in treating infections brought on by these strains. In this context, effective preventive and control measures should be implemented. One of the effective preventive measures is to application of limited antimicrobial drugs in seafood that have been recommended to curb the spread of Salmonella infection. The utilization of recent and new innovative technology to trace and eliminate Salmonella at each step of supply chains, including seafood processing, handling and preservation, can be recommended. One of the significant steps to its control is implementing a powerful level of cooperation and funding between health authorities and different nations, which is necessary from the human health perspective.
Conflict of Interest
The authors declare that there is no conflict of interest that could impact or influence the research work reported in this manuscript.
References
- Sodagari HR, Wang P, Robertson I, Habib I, Sahibzada S. Non-typhoidal Salmonella at the human-food-of-animal-origin interface in Australia. Animals. 2020;10(7):1192.
- Prabhakar P, Lekshmi M, Ammini P, Nayak BB, Kumar S. Salmonella contamination of seafood in landing centers and retail markets of Mumbai, India. Journal of AOAC International. 2020;103(5):1361-5.
- Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bulletin of the World Health Organization. 2004;82(5):346-53.
- Helms M, Ethelberg S, Mølbak K, DT104 Study Group. International Salmonella typhimurium DT104 infections, 1992–2001. Emerging infectious diseases. 2005;11(6):859.
- Mkangara M. Prevention and control of human Salmonella enterica infections: An implication in food safety. International Journal of Food Science. 2023;2023(1):8899596.
- Dekker J, Frank K. Salmonella, Shigella and yersinia. Clinics in laboratory medicine. 2015;35(2):225.
- Acheson D, Hohmann EL. Nontyphoidal salmonellosis. Clinical Infectious Diseases. 2001;32(2):263-9.
- Hendriksen RS, Vieira AR, Karlsmose S, Lo Fo Wong DM, Jensen AB, et al. Global monitoring of Salmonella serovar distribution from the World Health Organization Global Foodborne Infections Network Country Data Bank: results of quality assured laboratories from 2001 to 2007. Foodborne Pathogens and Disease. 2011;8(8):887-900.
- Iwamoto M, Ayers T, Mahon BE, Swerdlow DL. Epidemiology of seafood-associated infections in the United States. Clinical Microbiology Reviews. 2010;23(2):399-411.
- Heredia N, García S. Animals as sources of food-borne pathogens: A review. Animal Nutrition. 2018;4(3):250-5.
- Heinitz ML, Ruble RD, Wagner DE, Tatini SR. Incidence of Salmonella in fish and seafood. Journal of Food Protection. 2000;63(5):579-92.
- Amagliani G, Brandi G, Schiavano GF. Incidence and role of Salmonella in seafood safety. Food Research International. 2012;45(2):780-8.
- Centers for Disease Control (CDC. Iguana-associated salmonellosis–Indiana, 1990. MMWR. Morbidity and Mortality Weekly Report. 1992;41(3):38-9.
- Goldrick B. Emerging infections: Food borne diseases. Am.J Nurs. 2014;103:105-6.
- Spector MP. The Starvation-Stress Response (SSR) of Salmonella. Advances in Microbial Physiology. 1998;40:233-79.
- Feldhusen F. The role of seafood in bacterial food borne diseases. Microbes and Infection. 2000;2(13):1651-60.
- Liu X, Chen Y, Wang X, Ji R. Foodborne disease outbreaks in China from 1992 to 2001 national foodborne disease surveillance system. Journal of Hygiene Research. 2004;33(6):725-7.
- Liu XM, Chen Y, Guo YC, Wang ZT. Foodborne diseases outbreaks in 2005- report of National Foodborne Diseases Surveillance Network in China. Chin J Food Hyg. 2008;20:506-9.
- Naylor RL, Kishore A, Sumaila UR, Issifu I, Hunter BP, Belton B, et al. Blue food demand across geographic and temporal scales. Nature Communications. 2021;12(1):5413.
- Witte W. Medical consequences of antibiotic use in agriculture. Science. 1998;279(5353):996-7.
- Angulo FJ, Johnson KR, Tauxe RV, Cohen Ml. Origins and consequences of antimicrobial-resistant nontyphoidal Salmonella: implications for the use of fluoroquinolones in food animals. Microbial Drug Resistance. 2000;6(1):77-83.
- White DG, Zhao S, Sudler R, Ayers S, Friedman S, Chen S, McDermott PF, McDermott S, Wagner DD, Meng J. The isolation of antibiotic-resistant Salmonella from retail ground meats. New England J Medicine. 2001;345(16):1147-54.
- Cabello FC. Heavy use of prophylactic antibiotics in aquaculture: A growing problem for human and animal health and for the environment. Environmental Microbiology. 2006;8(7):1137-44.
- Zhao S, Datta AR, Ayers S, Friedman S, Walker RD, White DG. Antimicrobial-resistant Salmonella serovars isolated from imported foods. International journal of Food Microbiology. 2003;84(1):87-92.
- Sapkota A, Sapkota AR, Kucharski M, Burke J, McKenzie S, Walker P, Lawrence R. Aquaculture practices and potential human health risks: Current knowledge and future priorities. Environment International. 2008;34(8):1215-26.
- Organización de las Naciones Unidas para la Agricultura y la Alimentación. Fishery and Aquaculture Statistics: 2010. FAO. 2012.
- Su L, Chiu CH. Salmonella: clinical importance and evolution of nomenclature. Chang Gung Medical Journal. 2007;30(3):210.
- García-Fernández A, Fortini D, Veldman K, Mevius D, Carattoli A. Characterization of plasmids harbouring qnrS1, qnrB2 and qnrB19 genes in Salmonella. Journal of Antimicrobial Chemotherapy. 2009;63(2):274-81.
- Strohl WA, Rouse H, Fisher BD. Microbiologia ilustrada. Artmed. 2004.
- Angulo F. Antimicrobial agents in aquiculture: potential impact in public health. Enfermedades Infecciosas y Microbiología. 2000;20(6):217-9.
- Murugkar HV, Rahman H, Kumar A, Bhattacharyya D. Isolation, phage typing and antibiogram of Salmonella from man and animals in northeastern India. Indian Journal of Medical Research. 2005;122(3):237.
- Aragaw K, Molla B, Muckle A, Cole L, Wilkie E, Poppe C, et al. The characterization of Salmonella serovars isolated from apparently healthy slaughtered pigs at Addis Ababa abattoir, Ethiopia. Preventive veterinary medicine. 2007;82(3-4):252-61.
- Gebreyes WA, Davies PR, Morrow WM, Funk JA, Altier C. Antimicrobial resistance of Salmonella isolates from swine. Journal of Clinical Microbiology. 2000;38(12):4633-6.
- Acha PN. Zoonoses and communicable diseases common to man and animals. Pan American Health Org. 2001.
- Colquhoun J, Weetch RS. Resistance to chloramphenicol developing during treatment of typhoid fever. Lancet. 1950;2:621-3.
- Bhutta ZA. Current concepts in the diagnosis and treatment of typhoid fever. BMJ. 2006;333(7558):78-82.
- Zaki SA, Karande S. Multidrug-resistant typhoid fever: A review. The Journal of Infection in Developing Countries. 2011;5(05):324-37.
- Kumar R, Gupta N, Shalini. Multidrug-resistant typhoid fever. The Indian Journal of Pediatrics. 2007;74:39-42.
- Elhadi N. Prevalence and antimicrobial resistance of Salmonella spp. in raw retail frozen imported freshwater fish to Eastern Province of Saudi Arabia. Asian Pacific Journal of Tropical Biomedicine. 2014;4(3):234-8.
- Montenegro MA, Morelli G, Helmuth R. Heteroduplex analysis of Salmonella virulence plasmids and their prevalence in isolates of defined sources. Microbial Pathogenesis. 1991;11(6):391-7.
- Levy SB. Factors impacting on the problem of antibiotic resistance. Journal of Antimicrobial Chemotherapy. 2002;49(1):25-30.
- Rotger R, Casadesús J. The virulence plasmids of Salmonella. International Microbiology. 1999;2:177-84.
- Bäumler AJ, Tsolis RM, Ficht TA, Adams LG. Evolution of host adaptation in Salmonella enterica. Infection and Immunity. 1998;66(10):4579-87.
- Gulig PA, Doyle TJ. The Salmonella typhimurium virulence plasmid increases the growth rate of salmonellae in mice. Infection and Immunity. 1993;61(2):504-11.
- Guiney DG, Fang FC, Krause M, Libby S, Buchmeier NA, Fierer J, et al. Biology and clinical significance of virulence plasmids in Salmonella serovars. Clinical infectious diseases. 1995;21(2):S146-51.
- Boyd EF, Hartl DL. Salmonella virulence plasmid: Modular acquisition of the spv virulence region by an F-plasmid in Salmonella enterica subspecies I and insertion into the chromosome of subspecies II, IIIa, IV and VII isolates. Genetics. 1998;149(3):1183-90.
- Ahmer BM, Van Reeuwijk J, Timmers CD, Valentine PJ, Heffron F. Salmonella typhimurium encodes an SdiA homolog, a putative quorum sensor of the LuxR family, that regulates genes on the virulence plasmid. Journal of Bacteriology. 1998;180(5):1185-93.
- Bäumler AJ, Tsolis RM, Bowe FA, Kusters JG, Hoffmann S, Heffron F. The pef fimbrial operon of Salmonella typhimurium mediates adhesion to murine small intestine and is necessary for fluid accumulation in the infant mouse. Infection and Immunity. 1996;64(1):61-8.
- Muñoz-López M, García-Pérez JL. DNA transposons: Nature and applications in genomics. Current Genomics. 2010;11(2):115-28.
- Liebert CA, Hall RM, Summers AO. Transposon Tn 21, flagship of the floating genome. Microbiology and Molecular Biology Reviews. 1999;63(3):507-22.
- Pezzella C, Ricci A, DiGiannatale E, Luzzi I, Carattoli A. Tetracycline and streptomycin resistance genes, transposons and plasmids in Salmonella enterica isolates from animals in Italy. Antimicrobial Agents and Chemotherapy. 2004;48(3):903-8.
- Towner KJ. Bacterial genetics. InMedical Microbiol. 2012;69-81.
- Dalsgaard A, Forslund A, Petersen A, Brown DJ, Dias F, Monteiro S, et al. Class 1 integron-borne, multiple-antibiotic resistance encoded by a 150-kilobase conjugative plasmid in epidemic Vibrio cholerae O1 strains isolated in Guinea-Bissau. Journal of Clinical Microbiology. 2000;38(10):3774-9.
- Khan AA, Cheng CM, Van KT, West CS, Nawaz MS, Khan SA. Characterization of class 1 integron resistance gene cassettes in Salmonella enterica serovars Oslo and Bareily from imported seafood. Journal of Antimicrobial Chemotherapy. 2006;58(6):1308-10.
- Recchia GD, Hall RM. Gene cassettes: a new class of mobile element. Microbiology. 1995141(12):3015-27.
- Fluit AC, Schmitz FJ. Resistance integrons and super-integrons. Clinical Microbiology and Infection. 2004;10(4):272-88.
- Rådström P, Bäckman A, Qian NY, Kragsbjerg P, Påhlson C, Olcén P. Detection of bacterial DNA in cerebrospinal fluid by an assay for simultaneous detection of Neisseria meningitidis, Haemophilus influenzae and streptococci using a seminested PCR strategy. Journal of Clinical Microbiology. 1994;32(11):2738-44.
- Castro-Vargas RE, Herrera-Sánchez MP, Rodríguez-Hernández R, Rondón-Barragán IS. Antibiotic resistance in Salmonella spp. isolated from poultry: A global overview. Veterinary World. 2020;13(10):2070.
- Ugboko H, De N. Mechanisms of Antibiotic resistance in Salmonella typhi. Int J Curr Microbiol App Sci. 2014;3(12):461-76.
- Silva C, Wiesner M, Calva E. The importance of mobile genetic elements in the evolution of Salmonella: Pathogenesis, antibiotic resistance and host adaptation. Salmonella-A Diversified Superbug. 2012;231:254.
- Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiology and Molecular Biology Reviews. 2010;74(3):417-33.
- Carattoli A. Plasmid-mediated antimicrobial resistance in Salmonella enterica. Current Issues in Molecular Biology. 2003;5(4):113-22.
- Sirot D, Sirot J, Labia R, Morand A, Courvalin P, Darfeuille-Michaud A, et al. Transferable resistance to third-generation cephalosporins in clinical isolates of Klebsiella pneumoniae: Identification of CTX-1, a novel β-lactamase. Journal of Antimicrobial Chemotherapy. 1987;20(3):323-34.
- Domingues S, da Silva GJ, Nielsen KM. Integrons: Vehicles and pathways for horizontal dissemination in bacteria. Mobile Genetic Elements. 2012;2(5):211-23.
- Velge P, Cloeckaert A, Barrow P. Emergence of Salmonella epidemics: The problems related to Salmonella enterica serotyp Enteritidis and multiple antibiotic resistance in other major serotypes. Veterinary Research. 2005;36(3):267-88.
- Griggs DJ, Gensberg K, Piddock LJ. Mutations in gyrA gene of quinolone-resistant Salmonella serotypes isolated from humans and animals. Antimicrobial Agents and Chemotherapy. 1996;40(4):1009-13.
- Wong MH, Chan EW, Liu LZ, Chen S. PMQR genes oqxAB and aac (6′) Ib-cr accelerate the development of fluoroquinolone resistance in Salmonella typhimurium. Frontiers in Microbiology. 2014;5:521.
- Hur J, Jawale C, Lee JH. Antimicrobial resistance of Salmonella isolated from food animals: A review. Food Research International. 2012;45(2):819-30.
- Blair JM, Webber MA, Baylay AJ, Ogbolu DO, Piddock LJ. Molecular mechanisms of antibiotic resistance. Nature Reviews Microbiology. 2015;13(1):42-51.4
- Gray JT, Hungerford LL, Fedorka-Cray PJ, Headrick ML. Extended-spectrum-cephalosporin resistance in Salmonella enterica isolates of animal origin. Antimicrobial Agents and Chemotherapy. 2004;48(8):3179-81.
- Shaikh S, Fatima J, Shakil S, Rizvi SM, Kamal MA. Antibiotic resistance and extended spectrum beta-lactamases: Types, epidemiology and treatment. Saudi J Biological Sciences. 2015;22(1):90-101.
- Wu H, Wang Y, Wu Y, Qiao J, Li H, Zheng S, et al. Emergence of β-lactamases and Extended-Spectrum Β-Lactamases (ESBLs) producing Salmonella in retail raw chicken in China. Foodborne Pathogens and Disease. 2015;12(3):228-34.
- Bradford PA. Extended-Spectrum Β-Lactamases in the 21st century: characterization, epidemiology and detection of this important resistance threat. Clinical Microbiology Reviews. 2001;14(4):933-51.
- Tzouvelekis LS, Tzelepi E, Tassios PT, Legakis NJ. CTX-M-type β-lactamases: An emerging group of extended-spectrum enzymes. Int J Antimicrobial Agents. 2000;14(2):137-42.
- Bush K, Jacoby GA, Medeiros AA. A functional classification scheme for beta-lactamases and its correlation with molecular structure. Antimicrobial Agents and Chemotherapy. 1995;39(6):1211-33.
- Seiffert SN, Perreten V, Johannes S, Droz S, Bodmer T, Endimiani A. OXA-48 carbapenemase-producing Salmonella enterica serovar Kentucky isolate of sequence type 198 in a patient transferred from Libya to Switzerland. Antimicrobial Agents and Chemotherapy. 2014;58(4):2446-9.
- Miriagou V, Tassios PT, Legakis NJ, Tzouvelekis LS. Expanded-spectrum cephalosporin resistance in non-typhoid Salmonella. Int J Antimicrobial Agents. 2004;23(6):547-55.
- Hanson ND, Moland ES, Hossain A, Neville SA, Gosbell IB, Thomson KS. Unusual Salmonella enterica serotype Typhimurium isolate producing CMY-7, SHV-9 and OXA-30 β-lactamases. Journal of Antimicrobial Chemotherapy. 2002;49(6):1011-4.
- Alcaine SD, Warnick LD, Wiedmann M. Antimicrobial resistance in nontyphoidal Salmonella. Journal of Food Protection. 2007;70(3):780-90.
- Levy SB. Antimicrobial resistance: Bacteria on the defence. BMJ. 1998;317(7159):612-3.
- Li XZ, Nikaido H. Efflux-mediated drug resistance in bacteria: An update. Drugs. 2009;69:1555-623.
- Roberts MC, Schwarz S. Tetracycline and phenicol resistance genes and mechanisms: Importance for agriculture, the environment and humans. J Environmental Quality. 2016;45(2):576-92.
- McDermott PF, Tyson GH, Kabera C, Chen Y, Li C, Folster JP, et al. Whole-genome sequencing for detecting antimicrobial resistance in nontyphoidal Salmonella. Antimicrobial Agents and Chemotherapy. 2016;60(9):5515-20.
- Gilmore BF, Denyer SP, editors. Hugo and Russell’s pharmaceutical microbiology. John Wiley and Sons. 2023.
- Schwarz S, Kehrenberg C, Doublet B, Cloeckaert A. Molecular basis of bacterial resistance to chloramphenicol and florfenicol. FEMS Microbiology Reviews. 2004;28(5):519-42.
- Brands DA, Billington SJ, Levine JF, Joens LA. Genotypes and antibiotic resistance of Salmonella Newport isolates from US market oysters. Foodbourne Pathogens and Disease. 2005;2(1):111-4.
- Khan AA, Ponce E, Nawaz MS, Cheng CM, Khan JA, West CS. Identification and characterization of class 1 integron resistance gene cassettes among Salmonella strains isolated from imported seafood. Applied and Environmental Microbiology. 2009;75(4):1192-6.
- Kumar S, Lekshmi M, Parvathi A, Nayak BB, Varela MF. Antibiotic resistance in seafood‐borne pathogens. Foodborne Pathogens and Antibiotic Resistance. 2016:397-415.
- Boinapally K, Jiang X. Comparing antibiotic resistance in commensal and pathogenic bacteria isolated from wild-caught South Carolina shrimps vs. farm-raised imported shrimps. Canadian J Microbiology. 2007;53(7):919-24.
- Deekshit VK, Kumar BK, Rai P, Srikumar S, Karunasagar I, Karunasagar I. Detection of class 1 integrons in Salmonella Weltevreden and silent antibiotic resistance genes in some seafood‐associated nontyphoidal isolates of Salmonella in south‐west coast of India. Journal of Applied Microbiology. 2012;112(6):1113-22.
- Bouchrif B, Paglietti B, Murgia M, Piana A, Cohen N, Ennaji MM, et al. Prevalence and antibiotic-resistance of Salmonella isolated from food in Morocco. The Journal of Infection in Developing Countries. 2009;3(01):035-40.
- Onmaz NE, Abay S, Karadal F, Hizlisoy H, Telli N, Al S. Occurence and antimicrobial resistance of Staphylococcus aureus and Salmonella spp. in retail fish samples in Turkey. Marine Pollution Bulletin. 2015;90(1-2):242-6.
- Kuang D, Zhang J, Xu X, Shi W, Chen S, Yang X, et al. Emerging high-level ciprofloxacin resistance and molecular basis of resistance in Salmonella enterica from humans, food and animals. Int J Food Microbiology. 2018;280:1-9.
- Kotian A, Aditya V, Jazeela K, Karunasagar I, Karunasagar I, Deekshit VK. Effect of bile on growth and biofilm formation of non-typhoidal Salmonella serovars isolated from seafood and poultry. Research in Microbiology. 2020;171(5-6):165-73.
- Prabhakar P, Lekshmi M, Ammini P, Nayak BB, Kumar S. Serovar distribution, virulence gene and antibiotic susceptibility profiling of Salmonella enterica isolated from seafood in Mumbai, India. Microbial Pathogenesis. 2025:107530.
Author Info
Parmanand Prabhakar1*, Sanath Kumar H2, Pooja Saklani1, Srinu Rathlavath3, Md. Aman Hassan1, Sarvendra Kumar1
1College of Fisheries (Bihar Animal Sciences University), Kishanganj, Bihar, India
2Quality control laboratory, ICAR-Central Institute of Fisheries Education, Mumbai, India
3College of Fisheries Science, Uttar Pradesh Pandit Deen Dayal Upadhyaya Pashu Chikitsa Vigyan Vishwavidyalaya Evam Go-Anusandhan Sansthan (DUVASU), Mathura 281001, India
*Correspondence author: Parmanand Prabhakar, College of Fisheries (Bihar Animal Sciences University), Kishanganj, Bihar, India; Email: [email protected]
Copyright
Parmanand Prabhakar1*, Sanath Kumar H2, Pooja Saklani1, Srinu Rathlavath3, Md. Aman Hassan1, Sarvendra Kumar1
1College of Fisheries (Bihar Animal Sciences University), Kishanganj, Bihar, India
2Quality control laboratory, ICAR-Central Institute of Fisheries Education, Mumbai, India
3College of Fisheries Science, Uttar Pradesh Pandit Deen Dayal Upadhyaya Pashu Chikitsa Vigyan Vishwavidyalaya Evam Go-Anusandhan Sansthan (DUVASU), Mathura 281001, India
*Correspondence author: Parmanand Prabhakar, College of Fisheries (Bihar Animal Sciences University), Kishanganj, Bihar, India; Email: [email protected]
Copyright© 2025 by Prabhakar P, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Citation: Prabhakar P, et al. Molecular Mechanisms of Antibiotic Resistance in Seafood-Associated Salmonella Enterica: A Brief Review. J Clin Immunol Microbiol. 2025;6(1):1-10.