Occlusal Plane Dictated Skeletal and Dental Malocclusion with Concomitant Postural Diagnostic Findings-A Pilot Study Using Functional Positioning Overlays
Ogliara F1,3, Bagnasacco A1, Greven M2,3*
1- Private Office, Biella, Italy
2- Private Office, Bonn, Germany
3- University Dental School, Department of Prosthodontics, Medical University of Vienna, Austria
*Corresponding Author: Markus Greven, University Dental School, Department of Prosthodontics, Medical University of Vienna, Austria; Tel: +49-228985900; Email: markusgreven@t-online.de
Citation: Greven M, et al. Occlusal Plane Dictated Skeletal and Dental Malocclusion with Concomitant Postural Diagnostic Findings-A Pilot Study Using Functional Positioning Overlays. J Clin Med Res. 2020;1(2):1-17.
Copyright© 2020 by Greven M, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 04 May, 2020 | Accepted 25 May, 2020 | Published 01 Jun, 2020 |
Abstract
Objective: Aim of this investigation is to find evidence that the correction of the class II malocclusion and/or deep bite in children with mix dentitions using Functional Positioning Overlays (FPO) is faster and more stable than traditional approach and associated with an improvement in head posture and cervical spine.
Material and Method: Twenty patients (aged of the patients ranged from 6 to 9 years, mean age 7.5 years) presenting a dental class II occlusion
1) Underwent to preliminary instrumental evaluation: photos, models, cephalometrics and condilography (cadiax compact), GPA (Global Postural Analysis)
2) They were divided in two homogeneous groups (matching by age and sex)
- Ten patients were treated with acrylics crowns FPO (Functional Position Overlay) according to German Patent Number 10 2005 052 068 (2014) (similar to table tops)
- Ten patients were treated only with traditional treatment (fixed)
3) Instrumental revaluation was performed: after 7-8 months from the beginning of the therapy and at the end of the therapy
Results: A more rapid improvement in the mandibular adaptation (SNB/SND) was found in the cases treated with FPO than traditional approach; a more marked tendency to normalization was found in the values concerning cranio-cervical cephalometry and more quickly reach normality in the distribution of weight at level of the feet in patients treated with FPO that group control.
Conclusion: The results obtained demonstrated a tendency to reach faster the correction of the malocclusion in association with the improvement of the posture. The results are most likely related to the fact that FPO acts 24 hours a day on the mandibular position in growing patients.
Keywords
Class II malocclusion; Cephalometric X-ray; Orthodontic Therapy; Condylography
Introduction
Several dental orthodontic treatments have been suggested to correct Class II malocclusions [1]. Some treatments aim to move the upper front teeth backwards (with or without extraction of the teeth) whilst others aim to modify the growth of the upper or lower jaw or both to reduce the prominence of the upper front teeth. Treatment can involve the use of one or more types of orthodontic appliances. Some appliances apply a force directly to the teeth can either be removed from the mouth or fixed to the teeth during treatment. Other types of appliances are attached, via the teeth, to extraoral devices (e.g. headgear) that allow a force to be applied to the teeth and jaws via elastic bands to the posterior part of the head or neck. Treatment is usually carried out either early (early treatment), when a mixture of deciduous and adult permanent deciduous teeth are present (around 7 to 11 years of age) or later (adolescent adult treatment) after all the permanent teeth have erupted into the oral cavity (around 12 to 16 years of age). In severe cases and some adults, orthodontic treatment is suggested to be combined with orthognathic surgery to correct the position of one or both jaws.
From 2 to 14 years old the skeletal components growing within the craniofacial complex system interact with each other keeping a functional and structural balance whereas they increase in size during development [2]. The bone modelling activity are also observed in the human mandible during this postnatal period, the mandibular ramus shows a complex modelling pattern indicating a posterior growth of the mandible and its anterior displacement [2,3].
Our clinical practice, is based on the idea that the correction of malocclusion (class II) necessarily passes through mandibular forward advancement (articular compensation).
In the period of maturation of the masticatory organ and adolescence-hoodtes, articular compensation is the most essential factor in the final development of the occluso-articular relationship.
To a minimal and individual variable extent, the Temporomandibular Joints (TMJs) are capable of adapting to altered conditions during whole life.
In the first period the mandible is stabilized by the bilaminar zone (retro-articular cushion) which, being a rich vessel complex, swells and maintains the condyle and of course the mandible in a forward position.
Nature adapts and compensates to achieve optimum function.
Currently, a wide variety of functional devices is available in order to achieve forward growth of the jaw. Cozza et al., in 2006 published a systematic review of literature to evaluate the scientific evidence on the efficiency of functional devices in stimulating mandibular growth in patients with Class II malocclusion [4]. It turned out that different functional devices require different treatment times with different duration to obtain the Class II correction result at the occlusal level [5,6]. The average displacement for functional orthopedics of the jaws is 0.16 mm per month, with an average treatment duration of 17 months. Moreover, attention is drawn to the difficulty of obtaining a precise correction of malocclusion and, above all, the review highlighted the strict need to obtain good compliance by the patient. A non-adherent patient is indeed a guarantee of therapeutic failure. In order to solve the question about precision and patient’s compliance, we decided to use an orthodontic appliance that consisted in the creation of overlays to be applied on deciduous teeth that through the modification of the occlusion allows an immediate mandibular adaptation.
Backgrounds
The relationship between malocclusion and body posture is a controversial topic and still much debated in the scientific field. The last document of the Italian Society of Orthodontics (SIDO) states that, based on the review of the literature regarding head and body posture and occlusion, although some associations between occlusal features and posture alterations have been found, there is no scientific evidence that support a cause-effect relationship [7]. Most of the studies fall short in the methodology due to the lack of control groups, for the inappropriateness of the study project, for the poor validity and reproducibility of the diagnostic tests used. On the basis of these considerations it is not considered advisable to perform occlusal and/or orthodontic therapies, to treat or prevent alterations of posture or deviations of the spine [7].
It is therefore difficult, if not impossible, to establish an occluso-postural diagnosis protocol based on the investigation criteria examined so far. However, it is necessary to remember that the stomatognathic apparatus has interconnection with other systems such as respiratory, digestive, visual, vestibular, locomotor, auditory and that they can have a mutual influence [8-11].
On the basis of the data available from literature, significant associations were found between variables concerning head posture and craniofacial morphology [7-12].
It is a common clinical observation that predefined patterns of posture are created according to the occlusal classes. In fact, if in class II patients the physiological curves of the spine (cervical/lumbar lordosis and dorsal kyphosis) are in the correct position, in patients with class II it is noted that the presence of retrognathism is accompanied by an increase in lordosis due to the extension of the head. On the contrary, in patients with class III, due to the accentuated prognathism, we will witness the inverse situation in which the curves of the column progressively tend to decrease their angles.
To support these observations, some data are reported in literature. In 2005, D’Attilio et al., found significant differences among three different skeletal classes regarding the values of the inclination of the lower segment of the spinal column (EVT) to a true vertical (VER) [13]. EVT/VER angle was smaller (as absolute value) in class III than in skeletal class I and class II subjects (P < 0.001). More important, the angle created between the head and the midsection of the spinal column (Cervical lordosis angle – CVT/EVT) showed significant differences among the three groups.
Subjects in skeletal class II showed a significantly more extended head upon the spinal column than subjects in skeletal Classes I and III (P < 0.001 and P < 0.01, respectively). Evaluating differences among skeletal class I, class II, and class III subjects reported that cervical spine was significantly straighter in skeletal class III subjects (P ≤ 0.001). This study also revealed that a more lordotic curve of the spine was related to greater extension of the head and, additionally, to a skeletal class II (P ≤ 0.01). This increase in cervical lordosis, caused by the extension of the head, is supposed to be dictated by the need to make the first airways tract more open, increasing its functional capacity.
In our clinical practice, we observed that the position of the skull in cephalometry, in patients affected by class II malocclusion subjected to FPO treatment, tends to reach the correct position (reducing its extension and consequently correcting the cervical lordosis) in proportion to mandibular adaptation.
The mandibular advancement allows an enlargement of the first airways and reduces the need to hyper-extend the head [14]. Correction of the posture of the cervical spine appeared to be directly proportional to the advancement of the mandible: the faster the mandibular adaptation, the faster the improvement in posture (Fig. 1 and 2).
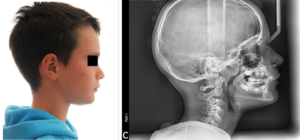
Figure 1: (a) Facial profile photography; (b) Lateral cephalometric x-ray before treatment.
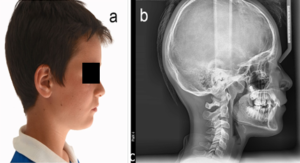
Figure 2: (a) Facial profile photography (b) Lateral cephalometric x-ray after treatment.
The systematic observation of these changes suggested the hypothesis of this study: using a combination treatment approach in early mixed dentition of skeletal class II low-angle and normo-angle deep bite configuration of FPO and 2×4 utility arch mechanics provides a more precise and faster adaptation of cranial-mandibular system than traditional orthodontic method.
The mechanisms that make it possible to obtain that are: occlusal plane correction (flattening), vertical support, retrusive guide, no interference.
Modifying the original idea of Prof. Sato, we decided to use composite materials to build FPO instead of the original metal [15-21]. Applying the concepts of prof. Salvicek regarding dental occlusion, we perform a sequential wax-up of class II on patient models, working on the occlusal surfaces of the superior and inferior deciduous molars [15-17]. The data regarding the cranial anatomy and the articular functionality of the patients are obtained through the cephalometric study of lateral cranial radiography and condylography. The VTO feature -GAMMA dental software (Fig. 3) is used to previsualize the mandible movement on SCI (Sagittal Condylar Inclination).
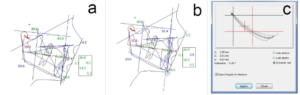
Figure 3: Visiualiuzed Treatment Objective (VTO) (Cadias, Gamma Dental Software, Klosterneuburg, Austria): a) Cephalometric tracing with overlayed jaw motion tracking (Cadiax, Gamma Dental Software, Klosterneuburg, Austria); b) Cephalometric tracing visualizing anterior mandibular Therapeutic Position (ThP); c) Precision Planning-Window of anterior mandibular Therapeutic Position (ThP) (Cadias, Gamma Dental Software, Klosterneuburg, Austria).
The systematic and combined use of these tests allows an accurate setting of the articulator (CPV) and therefore the possibility of performing a correct waxing. The models are mounted in maximum intercuspidation. When little patients aren’t collaborating or in the position of maximum retrusion of the non-forced mandible, detected without dental contact. The inferior model is moved forward on the sagittal condylar inclination, to allow the first class with the condylar position movement articulator (CPV-Fig. 4a and 4b).
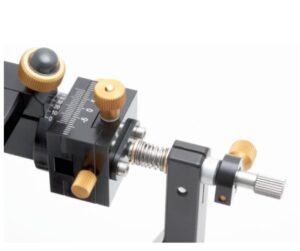
Figure 4a: Implementing / applying mandibular therapeutic position in Condylar movement/Position articulator/Variator (CPV) (Gamma Dental Software, Klosterneuburg, Austria).
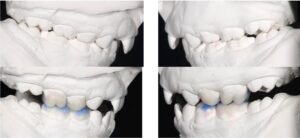
Figure 4b: Modell-situation lateral view right/left in articulated situation in “starting” position (upper pictures) and in mandibular Therapeutic Position (ThP) showing Functional Positioning Overlays (FPO) in the waxed-up situation.
The FPOs are poured into the patient’s mouth and glued like adhesive crowns. As previously mentioned, once positioned the FPO immediately start functioning, educating the jaw to adapt to the therapeutic position, without there being the need for any cooperation from the patient (Fig. 5a-5f).

Figure 5a: Intraoral photography right lateral view before treatment.
Figure 5b: Intraoral photography frontal view before treatment.

Figure 5c: Intraoral photography left lateral view before treatment.

Figure 5d: Intraoral photography right lateral view during treatment with applied FPOs in mandibular Therapeutic Position (ThP).

Figure 5e: Intraoral photography frontal view during treatment with applied FPOs in mandibular Therapeutic Position (ThP).

Figure 5f: Intraoral photography left lateral view during treatment with applied FPOs in mandibular Therapeutic Position (ThP).
This system also works 24 hours a day in all conditions. Likewise, once the therapeutic position is reached, the FPOs do not need to be removed as they are eliminated once the deciduous teeth are naturally lost. The new mandibular position will then be maintained by the occlusion of the permanent teeth.
In order for them to be effective, deciduous teeth and FPO, must remain for at least a year.
The aim of this investigation is to find evidence that the correction of the class II malocclusion and deep bite, in children with mixed dentition using FPO, is faster and long lasting efficient than traditional approach and associated to improvement of head and cervical spine position.
Materials and Methods
From January 2016 to December 2019, 20 young patients were enrolled for this study. All of them (13 girls and 7 males) were consecutively treated by the same operator. The age of the patients ranged from 6 to 9 years (mean age 7.5 years).
At the beginning, all individuals were divided in 2 homogeneous groups (matching by age and sex). The first group (10 patients) was treated with acrylics crowns Functional Position Overlay (FPO) according to German Patent Number 10-2005-052-068 (2014) and the use of a 2×4 utility arch when incisors don’t allow mandibular forward movement.
The second group (10 patients) was treated only with traditional fixed treatment (utility arch and class II elastics).
The following inclusion criteria were adopted:
- Mix dentitions (at least 4 deciduous teeth)
- Deciduous teeth should remain in the mouth for a minimum period of one year
- Class II occlusion; low or mesio angle, deep or normo bite
- Previously obtained informed consent to use patient data
The following exclusion criteria were adopted:
- High angle, open bite
- Full permanent dentitions.
Each patient underwent the following initial assessment:
- Clinical examination (muscle palpation, clinical evaluation of oral dysfunctions)
- Photographs of the patient (facial and oral)
- Study models (ICP bite, face bow)
- X-ray panoramic
- Cephalometrics (Cadias analysis – Gamma Dental Software)
- Condylography (Cadiax compact analisys – Gamma Dental Software)
- Postural measurement (Stabiloboard postural platform)
The methods used for the research were as follows:
- Clinical and instrumental re-evaluation were performed twice: the first one after 7/8 months from the beginning of the therapy and the second at the end of the therapy, and included cephalometry and postural analysis.
- All clinical evaluations were performed by the same operator.
- The natural position of the head was obtained by asking the patient to take two deep breaths before proceeding with the radiographic examination. All radiographs were obtained by only one operator using a X-rays One-shot Pax-i 2D (Vatech), operating at 80 kVp, 10 mA, 0.9 seconds of exposition and 1.50 m focal distance, with individuals in natural head position in all exposures.
- The cranio-cervical analysis was performed using the caphalometric points indicated by the following authors: Slaviceck, Sato, Steiner and Rocabado [23-26]. The following values have been taken into consideration for every assessments: Antero-posterior Displasia Indicator (APDI), Overbite Depth Indicator (ODI), Sella-Nasion B-point (SNB), Sella-Nasion D-point (SND), Cranio-Cervical Angle (CCA), Occiput-Atlas distance (OA) and Hyoid Triangle height (HT) [23-30]. These values were subsequently considered in the statistical analysis.
- Postural assessment was based on measuring the distribution of weight on the foot. Under normal conditions, the physiological curves of the spine determine a percentage distribution of weight on the level of the feet which was quantified by Kapandji in the following way: 50% on the hindfoot and 50% on the forefoot. The altered position of the cervical spine causes patients with second-class malocclusion to tend to carry most of their weight on the forefeet. Before every measurement, each patient was invited to step onto the platform and take two steps on the spot, keeping their eyes in a natural position. After correctly positioning the feet, the coordinates of each foot were recorded, which the patient could no longer change for the entire duration of the examination. Furthermore, before starting the recording, each patient was asked to perform two deep breaths so as to set the vertebral column in a natural position. In order to avoid any visual interference, all measurements were taken with the eyes closed. Each measurement was performed twice, the first with the mandible in rest position and the second with maximum Intercuspation (ICP). Each measurement lasted for 30 seconds.
The following technical equipment were used:
- Cephalostat One-shot Pax-i 2D (Vatech) operating with 80 kVp, 10 mA, 0.9 seconds of exposition, 1.50 m focal distance
- Condylograph and Cadiax Compact (Gamma dental, Austria)
- Reference SL articulator and CPV (Condilar Position Variator) Gamma dental, Austria
- Gamma dental software version 8.3.4 (Gamma dental, Austria)
- The Global Postural Analysis software (GPA) which follows the directives of the new regulations in force since 2015 and is certified according to the DDM 93/42 as a class I medical device certified by ISO 9001 and ISO 13485.
Results
Data collection ended in April 2019. No patients were excluded from the study and all completed orthodontic therapy.
The statistical analysis was performed by the Laboratory of Experimental Testing of the UDA of “Ortognatodonzia e Odontoiatria Infantile” of the Department of Clinical-Surgical, Diagnostic and Pediatric Sciences of the University of Pavia. The analysis was carried out with the software R (R version 3.1.3, R Development Core Team, R Foundation for Statistical Computing, Wien, Austria) calculating the statistics descriptive for each variable that included: average, standard deviation, median, minimum values and maximum, measured for each group (Fig. 6).

Figure 6: Treatment sequence intraoral photographs. Upper row: starting situation right, frontal, left and overbite/overjet view. Middle row: during treatment (8 months) with applied 2×4 utility arch upper jaw and FPOs right, frontal, left and overbite/overjet view. Bottom row: end of treatment (18 months) right, frontal, left and overbite/overjet view.
The normality of the distributions was evaluated by Kolmogorov and Smirnov test. Subsequently an ANOVA test was applied for repeated measurements followed by Tukey’s test as post-hoc (Fig. 7a and 7b).
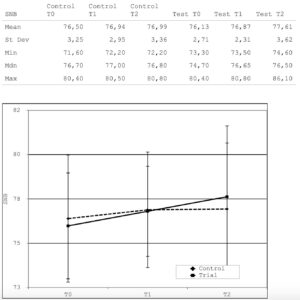
Figure 7a: Statistical evaluation showing the development of SNB-angle during treatment in patient-group and control group.
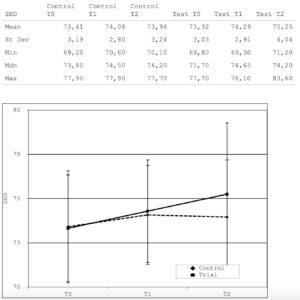
Figure 7b: Statistical evaluation showing the development of SND-angle during treatment in patient-group and control group.
For all the tests the significance was set for P <0.05.
An important premise must be made before the results are discussed.
It is clear that such a small number of cases is not good enough to reveal any statistical significance; twenty patients are too few in relation to the type of scientific study and the number of variables analyzed. We are aware of the fact that, in order to obtain results that have an effective statistical value, the number of cases to be considered should be at least one hundred individuals.
Despite the lack of significance, there are clearly identifiable trends that could very probably become significant by increasing the number of patients included in the study.
- The values SNB and SND showed a clearer and more rapid improvement in the group treated with FPO compared to the group treated with traditional fixed therapy. In particular, these last two values have shown a constant improvement trend throughout the duration of the therapy. Concerning the same values, the control group showed improvement only in the first half of therapy; in the second half, however, the trend remained constant on the values previously achieved. Since these last two values are important in assessing the prognostic growth trend of the mandible, it seems clear that the use of FPOs is useful in correcting the class II more quickly than the fixed therapy.
- The analysis of the values of cervical cephalometry, a more marked tendency to normalization was detected in patients undergoing treatment with FPO than the control group. This tendency was particularly evident in the values concerning the Cranio-Cervical Angle (CCA) and the height of the Hyoid Triangle (HT). An excess of correction has been noted in the value concerning the Occipital-Atlas distance (OA). This augmentation in distance could actually be linked to the rapid enlargement of the oral airspace due to the significant increase in the prognathism induced by the FPOs themselves. In this sense, the increase in OA could be considered almost a compensation mechanism in patients accustomed from birth to having a reduced OA, linked to the hyperextension of the head that they must maintain to promote correct breathing.
- The distribution of weight at the level of the feet, considering as normal the percentages indicated by Kapandij (50% on the front foot and 50% on the back foot), we observed that the tendency to more quickly reach normality is evident in the group of patients treated with FPO. This trend is stronger when comparing the recordings made during maximum Intercuspation (ICP).
The fact that the differences in weight distribution are smaller with the mandible in the resting position, leads to the conclusion that: by eliminating the visual component, the teeth can actually act as an organ of stability when the two arches are in contact with each other and in correct relationship.
Conclusion
The first conclusion we have drawn from this experience is that the study we presented in these pages is far from complete, in fact the follow up of all patients one year after the end of the therapy was not completed; however, we have been able to observe the maintenance of the result on most patients. The results obtained and discussed previously, even if without statistical significance, have nevertheless demonstrated unequivocal tendencies that lead us to continue with this research. Furthermore, the experience accumulated in this period with the use of FPO, in the treatment of class II cases and deep bite, has allowed us to ascertain their real clinical efficacy. Compared to traditional fixed therapy, the application of FPO can reduce treatment times associated with a significant decrease in patient discomfort. It is important to underline the fact that this kind of therapy practically erases the role of the child’s compliance, in fact the FPO constantly works during all 24 hours. Their application in the patients’ mouth does not cause particular difficulties in relation to the patient’s compliance and their removal occurs simply with the loss of deciduous teeth. The biggest difference compared to the fixed therapy is that the teeth on which the FPO are mounted, guide the mandible into the correct position.
References
- Batista KBSL, Thiruvenkatachari B, Harrison JE, O’Brien KD. Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents (Review). Cochrane Database of Systematic Reviews. 2018;3:CD003452.
- Enlow DH, Harris DB. A study of the postnatal growth of the human mandible. Am J Orthod Dentofacial Orthop. 1964;50(1):25-50.
- Kurihara S, Enlow DH, Rangel RD. Remodeling reversals in anterior parts of the human mandible and maxilla. Angle Orthod. 1980;50(2):98-106.
- Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara Jr JA. Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop. 2006;129(5):599.
- Santos-Pinto PR, Martins LP, Santos-Pinto AD, Gandini Júnior LG, Raveli DB, Santos-Pinto CC. Mandibular growth and dentoalveolar development in the treatment of Class II, division 1, malocclusion using Balters Bionator according to the skeletal maturation. Dent Press J Orthod. 2013;18(4):43-52.
- De Almeida MR, Henriques JF, Ursi W. Comparative study of the Fränkel (FR-2) and bionator appliances in the treatment of Class II malocclusion. Am J Orthod Dentofacial Orthop. 2002;121(5):458-66.
- Michelotti A, Buonocore G, Manzo P, Pellegrino G, Farella M. Dental occlusion and posture: an overview. Progress Orthod. 2011;12(1):53-8.
- Cai M, Brown EC, Hatt A, Cheng S, Bilston LE. Effect of head and jaw position on respiratory-related motion of the genioglossus. J Appl Physiol. 2016;120(7):758-65.
- Keersmaekers KD, De Boever JA, Van Den Berghe L. Otalgia in patients with temporomandibular joint disorders. J Prosthet Dent. 1996;75(1):72-6.
- Cuccia AM, Caradonna C. Binocular motility system and temporomandibular joint internal derangement: A study in adults. Am J Orthod Dentofacial Orthop. 2008;133(5):640.
- Vass Z, Shore SE, Nuttall AL, Miller JM. Direct evidence of trigeminal innervation of the cochlear blood vessels. Neuroscience. 1998;84(2):559-67.
- Gomes LD, Horta KO, Gonçalves JR, Santos-Pinto AD. Systematic review: craniocervical posture and craniofacial morphology. Euro J Orthod. 2014;36(1):55-66.
- An JS, Jeon DM, Jung WS, Yang IH, Lim WH, Ahn SJ. Influence of temporomandibular joint disc displacement on craniocervical posture and hyoid bone position. Am J Orthod Dentofacial Orthop. 2015;147(1):72-9.
- Armijo-Olivo S, Magee D. Cervical musculoskeletal impairments and temporomandibular disorders. J Oral Maxillofac Res. 2012;3(4):12.
- Sonnesen L. Associations between the cervical vertebral column and craniofacial morphology. Int J Dentistry. 2010;2010.
- D’Attilio M, Caputi S, Epifania E, Festa F, Tecco S. Evaluation of cervical posture of children in skeletal class I, II, and III. J Craniomandibular Prac. 2005;23(3):219-28.
- Ghodke S, Utreja AK, Singh SP, Jena AK. Effects of twin-block appliance on the anatomy of pharyngeal airway passage (PAP) in class II malocclusion subjects. Prog Orthod. 2014;15(1):68.
- Slavicek R. Gelenkpositionsdiagnostik: und gezielte initialtherapie mit aufbisschienen im unterkiefer. Dtsch Zahnärztl Z. 1980;35:616-20.
- Slavicek R, Die Funktionellen. Determinanten des kauorgans. zahnärztlich medizinisches schrifttum, München. 1984.
- Slavicek R, Lugner P. Uber die MOglichkeit der Bestimmung des Bennettwinkels bei sagittaler Aufzeichnung. Osterr Z Stomatol. 1978;75:270.
- Greven M, Reichardt G. Orthodontic early treatment during mixed dentition taking into consideration functional aspects avoiding removable orthodontic appliances MSc-Thesis DUK/KDU/Tufts University. 2003.
- Sato S. Early Treatment and preventive treatment of temporomandibular disorders and occlusion in adolescence. 2007;6:109-142.
- Sato H, Fujii T, Uetani M, Kitamori H. Anterior mandibular repositioning in a patient with temporomandibular disorders: a clinical and tomographic follow-up case report. Cranio. 1997;15(1):84-8.
- Sato S. A treatment approach to malocclusions under the consideration of craniofacial dynamics. Grace Printing Press. 1991.
- Steiner CC. Cephalometrics in clinical practice. Angle Orthod. 1959;29(1):8-29.
- Rocabado M. Biomechanical relationship of the cranial, cervical, and hyoid regions: a discussion. J Craniomandibular Prac. 1983;1(3):61-6.
- Kim YH, Vietas JJ. Anteroposterior dysplasia indicator: an adjunct to cephalometric differential diagnosis. Am J Orthod. 1978;73(6):619-33.
- KIM YH. A comparative cephalometric study of Class II, Division 1 nonextraction and extraction cases. Angle Orthod. 1979;49(2):77-84.
- Kim YH, Caulfield Z, Chung WN, Chang YI. Overbite depth indicator, anteroposterior dysplasia indicator, combination factor and extraction index. Int J MEAW. 1994;1(1):81-104.
- Kahn J, Tallents RH, Katzberg RW, Ross ME, Murphy WC. Prevalence of dental occlusal variables and intraarticular temporomandibular disorders: molar relationship, lateral guidance, and nonworking side contacts. J Prosthet Dent. 1999;82(4):410-5.
This work is licensed under Attribution-NonCommercial-NoDerivs 2.0 Generic (CC BY-NC-ND 2.0) International License. With this license readers are free to share, copy and redistribute the material in any medium or format as long as the original source is properly cited.

