Mohammad Haydar1,2*, Fadi Nasser1, Elliott Cohen1, Uriel Levinger1,2
1Internal Department C, Laniado Medical Center, Netanya, Israel
2Adelson School of Medicine at Ariel University, Israel
*Correspondence author: Mohammad Haydar, MD, Specialist physician, Laniado Netanya Medical Center, Internal Medicine Department, Israel; Email: [email protected]
Published Date: 23-04-2024
Copyright© 2024 by Haydar M, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Pleural effusion, the pathological accumulation of fluid in the pleural space, is very common. Its causes vary widely, ranging from fairly harmless effusions accompanying viral pleuritis to prognostically highly relevant ones due to congestive heart failure or malignances. Pleural effusions are classified by their biochemical properties into exudative and transudative effusions but can also be due to blood, pus and chyle. Applying Light’s criteria may be helpful to diagnose an exudative effusion.
Exudative effusions are commonly caused by infection, malignancy and inflammatory disorders, such as rheumatoid arthritis.
In this case we presented 39 women that was admentes with only short of breath and Pleural effusion, During the hospitalization, a pleural fluid puncture was performed and a cytological result was obtained for ovarian cancer and CA-125 was high in the pleural fluid, the patient underwent chemotherapy and her condition improved hourly.
In this case, we present a rare case in which the patient complained of shortness of breath without surgical or gynecological complaints and was finally diagnosed with ovarian cancer, which raises the importance of ruling out malignancy every time a new pleural fluid is aspirated.
Keywords: Pleural Effusion; Dyspnea; Ovarian Carcinoma; Internal Medicine; Oncology
Abbreviation
PE: Pleural Effusion; MPE: Malignant Pleural Effusions; OC: Ovarian Cancer; CT: Computed Tomography; ECG: Electrocardiogram
Introduction
Pleural Effusion (PE), the pathological accumulation of fluid in the pleural space, is very common finding clinically. Its causes vary widely, ranging from fairly harmless effusions accompanying viral pleuritis to prognostically highly relevant ones due to congestive heart failure or malignances [1]. Pleural effusions are classified by their biochemical properties into exudative and transudative effusions but can also be due to blood, pus and chyle (Table 1). Applying Light’s criteria may be helpful to diagnose an exudative effusion (Table 2) [2]. However, 25% of transudates are misclassified as exudative effusions and therefore, calculating the serum to pleural fluid albumin gradient may be necessary to avoid misdiagnosis [2]. Exudative effusions are commonly caused by infection, malignancy and inflammatory disorders, such as rheumatoid arthritis [2]. Malignant Pleural Effusions (MPE), more common in lung and breast malignancies, affect up to 15% patients with cancer [1].
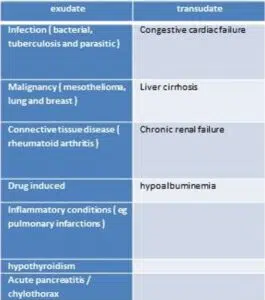
Table 1: Common causes of exudative and transudative pleural effusions.
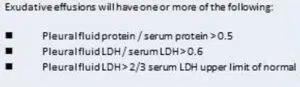
Table 2: Lights criteria for exudative effusions.
Case Report
A 39 years old woman presented to our institution, with a past medical history of iron deficiency anemia treated with iron pills and a previous hysteroscopy from one year prior that was normal. She was not taking any other regular medications or had any known allergies. She was admitted to the emergency room due to chest pains on the right side of the chest for a week. She described the pains as point-like in nature in the rib area on the posterior aspect on the right side of the chest. She further complained of shortness of breath, especially when lying on her back. There were no other complaints including: cough, fever, chills, fall, weight loss, night sweats, chest injury, gastrointestinal or urinary complaints. She attempted to alleviate her pain with over-the-counter analgesics, but they did not help. The patient’s vitals were pulse 104, no fever, saturation 98% on room air. E.K.G. showed regular sinus rhythm without signs of acute ischemia. On physical examination, air intake was reduced on the right side, without wheezing or crepitations. There was tenderness on palpation of the chest on the right in the lateral aspect in the 12th rib. A series of test were ordered to help elucidate the patient’s disease. A chest X-ray demonstrated a large amount of pleural fluid. A chest CT was performed and pulmonary embolism was ruled out. A large amount of pleural fluid was demonstrated on the right without evidence of pericardial fluid (Fig. 1). She was admitted to the internal department for further investigation and treatment.
In the Internal Medicine Department, a pleuralcentesis was performed. In calculating the values according to Light Criteria, the fluid was found to be exudative. To rule out an inflammatory and endocrine diseases that can be make a plural effusion in young people, a wide variety of investigations were performed: Anti-MPO = 0.8 IU/mL Anti-PR3 = 1.6 IU/mL Antinuclear antibodies screen = 0.3 ratio Rf = 15.8 IU/ml TSH 6.97 Uiu/Ml FT4 1.46 ng/Dl – all of them were within normal range. It was also decided to perform tests for malignant disease by taking a panel of tumor markers from the pleural fluid and from serum considering there were no signs infection in the initial work up. She was found to have elevated CA-125 in pleural effusion and serum of 11604 U/ml and 5114 U/ml, respectively. Pleural fluid cytology also demonstrated adenocarcinoma and was suggestive of breast/ovarian origin. Immunistains Ck7 and GATA3 positive. Calretinin, desmin and TTF1 were negative.
A total body CT was then performed, which demonstrated a nodule behind the ovary and caused an indentation on the right rectal wall (Fig. 1). There were also large lymph nodes on the right round ligament of the uterus. A hypodense plaque with two cystic nodules on the posterior margin of the liver were found as well. Suspected metastatic lesions were also found between the liver, the diaphragm and thick omental cake at the lower end of the greater omentum.
A biopsy was performed from the mass in the omentum which demonstrated High Gtade Serous Carcinoma. Later, the patient began follow-up and treatment at an oncology clinic. A standard neoadjuvant chemotherapy treatment with Keytruda + Carbotexol was as is recommended by the National Comprehensive Cancer Network. In addition, the patient was started on experimental new immunotherapies as part of a study that included MK4830 and MK 3475.
MK4830 is a first in class human IgG4 monoclonal antibody targeting the immunoglobulin – like transcript 4 receptor. MK 3475 Anti PD 1 monoclonal antibody(pembrolizumab).
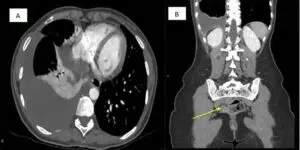
Figure 1: A: Large amount of pleural fluid was right side; B: Right ovary behind the uterus and causes an indentation on the right rectal wall.
Discussion
Malignancy is one of the most common causes of exudative and unilateral pleural effusion. Its incidence is increasing as cancer prevalence and life expectancy with newer cancer therapies have developed. In fact, 15% of all cancer patients will develop a pleural effusion [3]. Most malignant pleural effusions are due to metastatic lung cancer in men and metastatic breast cancer in women. Lung and breast cancer account for 50%-65% of all malignant pleural effusions [3]. Lymphoma accounts for approximately 10% of malignant pleural effusions, while ovarian and gastric cancer account for approximately 5% of malignant pleural effusions [3].
In our patient, she had a large unilateral plural effusion and a pleural puncture was performed, a large amount of oxidative fluid was obtained. Chest X-ray after the puncture showed no evidence of an inflammatory process. Laboratory investigation for autoimmune and inflammatory diseases were negative. It was then decided to rule out malignant causes of the exudative fluid using tumor markers. CA 125 was found and a total body CT scan demonstrated ovarian cancer with metastatic spread throughout her body.
Ovarian Cancer (OC) encompasses a heterogeneous group of malignancies, over 90% of which are of epithelial origin [4]. About half of patients with OC survive beyond five years after diagnosis, partly because more than 70% are discovered in an advanced disease stage [4]. The use of Computed Tomography (CT) has become standard practice to locate tumor deposits before primary tumor. Previous reports in the literature have identified CT findings that are considered to be indicators of whether a pleural effusion is malignant, such as pleural thickening greater than 1 cm and/or pleural nodularity and irregularity [3].
Pleural effusions in ovarian cancer have been reported to be moderate to large in size and are associated with enlarged superior diaphragmatic lymph nodes. The mechanism of metastatic pleural involvement in OC is speculative and probably includes one or more of the following: a) invasion from an affected contiguous diaphragm, b) migration of tumor cells from the peritoneal cavity to the pleural space through small diaphragmatic defects and c) hematogenous spread. The relevance of the first two potential ways of cancer dissemination was supported by the finding of ascites and peritoneal metastases (which encompasses peritoneal diaphragmatic implants) as independent predictors of PE development [3]. In our patient, the malignant cells of the ovary may have moved to pleura directly via the blood stream, leading to production of pleural effusion without producing ascites.
Massive pleural effusion is often caused by malignancy. It has been suggested that CA-125 titres (above 1000 U/ml) could differentiate benign from malignant conditions. CA-125 is a high molecular mass glycoprotein expressed on the cell surface of some derivatives of embryonic coelomic epithelium [5]. CA 125 is elevated in only 50% of women with early-stage disease and is detected in other benign gynecological conditions such as endometriosis, pregnancy, as well as nongynecological conditions as cirrhosis and congestive heart diseases. Serum CA-125 levels are increased in ovarian cancer and decrease after effective treatment.
In the case of our patient, the accuracy of CA-125 measurement in PE and serum was 11604 and 5114, respectively. Other authors report a 37% sensitivity and 100% specificity at a cutoff value of 1000 U/l.
Conclusion
One of the most important aspects in the process of investigating unilateral pleural fluid is to raise the suspicion of Malignant Pleural Effusion (MPE). Many patients with ovarian cancer develop a MPE throughout her illness. However, there are few studies that identify how many of them debut with a MPE as the first symptom of Gynecological malignancies. Furthermore, by analyzing the amount of CA- 125 found in the pleural fluid of a patient, this may help physicians to anticipate advancement of disease. For instance, a CA 125 of less than 1000 may indicate benign disease. We suggest that better understanding of pathophysiological mechanisms of MPE in the near future would promote better prognosis for patients with Ovarian CA.
Conflict of Interests
Authors declare that there is no conflict of interest for this paper.
Acknowledgements
We thank the patients and their families.
References
Case Report
Received Date: 24-03-2024
Accepted Date: 15-04-2024
Published Date: 23-04-2024
Copyright© 2024 by Haydar M, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Haydar M, et al. Plueral Effusion and Ovarian Cancer. J Neuro Onco Res. 2024;4(1):1-5.

Figure 1: A: Large amount of pleural fluid was right side; B: Right ovary behind the uterus and causes an indentation on the right rectal wall.

Table 1: Common causes of exudative and transudative pleural effusions.

Table 2: Lights criteria for exudative effusions.