Primary Cutaneous Cryptococcosis Caused by Cryptococcus neoformans in n Immunocompetent Patient
Jéssica Louise Benell1,2, Rossana Patrícia Basso1,3,4,5, Vanice Rodrigues Poester1,4,6, Lívia Munhoz Silveira4, Aline Barcellos Grill3,5, Luciano Zogbi Dias3,5,6, David A Stevens7, Melissa Orzechowski Xavier1,4,6*
1Laboratory of Mycology, Faculty of Medicine, Federal University of Rio Grande, Rio Grande, RS, Brazil
2Professor of Department of Diagnoses Methods of Federal University of Healthy Sciences of Porto Alegre (UFCSPA), Porto Alegre, RS, Brazil
3Universitary Hospital of Federal University of Rio Grande (HU-FURG/EBSERH), Rio Grande, RS, Brazil
4Postgraduate Program in Health Sciences, Faculty of Medicine, Federal University of Rio Grande, Rio Grande, RS, Brazil
5Specialized Care Service in Infectious Diseases at the Universitary Hospital of Federal University of Rio Grande (HU-FURG/EBSERH), Brazil
6Professor of Faculty of Medicine, Federal University of Rio Grande, Rio Grande, RS, Brazil
7California Institute for Medical Research, San Jose and Division of Infectious Diseases and Geographic Medicine, Stanford Univ. Medical School, Stanford, California, USA
*Correspondence author: Melissa Orzechowski Xavier. Laboratório de Micologia, Faculdade de Medicina, Universidade Federal do Rio Grande, Campus Saúde. Visconde de Paranaguá 102, Centro, 96201-900, Rio Grande, RS, Brazil; Email: melissaxavierfurg@gmail.com
Citation: Xavier MO, et al. Primary Cutaneous Cryptococcosis Caused by Cryptococcus neoformans in an Immunocompetent Patient. Jour Clin Med Res. 2023;4(2):1-4.
Copyright© 2023 by Xavier MO, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 10 Aug, 2023 | Accepted 24 Aug, 2023 | Published 31 Aug, 2023 |
Abstract
Background: Primary Cutaneous Cryptococcosis (PCC) is an uncommon disease restricted to cutaneous tissues caused by Cryptococcus spp. Case-report: We report a PCC case in a patient without any underlying disease. A 44-year-old man from Southern Brazil was referred to the hospital with 3-year recurrent skin lesions. A biopsy showed typical rounded and encapsulated blastoconidia typical of Cryptococcus and C. neoformans was identified in culture. Treatment with fluconazole (600 mg/day) was prescribed with improvement of the lesions. During the follow-up a self-reported interruption of treatment was detected and after 1 year of treatment, complete clinical cure was not yet achieved. Conclusion: This uncommon case reinforces the importance of mycologic examinations for correct diagnoses.
Keywords: Cryptococcosis; Cryptococcus Neoformans; Immunocompetent; Infectious Agents; Fungal Infections; Occupational Exposure
Introduction
Primary Cutaneous Cryptococcosis (PCC) is a manifestation restricted to cutaneous tissues. In 1972, Noble and Fajardo established three criteria for the diagnosis of PCC, which are current, being: a) absence of infection in other viscera, b) fungus isolation from the skin and c) absence of extracutaneous manifestations after 4 weeks of diagnostic efforts [1]. This less severe presentation of cryptococcosis is uncommon, with only 18 cases reported in 38 years and generally associated with a good outcome [2]. Skin lesions in PCC can occur as papules, pustules, nodules, ulcers, abscesses, plaques and/or even granulomas, localized mainly on the head and neck [3]. Although the inhalation of basidiospores or dessicated blastoconidia is the main route of systemic infection by Cryptococcus spp. the route of infection for PCC has not yet been fully clarified. It is suggested the disease can be induced by inoculation [1,4,5]. Here we report a PCC case in an immunocompetent patient, without underlying disease but with constant occupational exposure to the main source of infection for Cryptococcus spp.
Case Report
A man, 44-year-old, white, worker at a refinery in Rio Grande’s harbor, a port city in the extreme south of Brazil, was referred to the HU-FURG / EBSERH, in October 2020, with a three-year history of ulcerative and painful skin lesions on his face, chest and right forearm (D0). The patient had no other systemic symptoms and no history of any pulmonary abnormalities during this period. The patient reported several previous antibacterial treatments without more specific examinations for the diagnosis. He had not received any pharmacological treatment for the previous 8 months. Physical examination showed no fever or other systemic findings, no pulmonary symptoms and no lymphadenopathy or organomegaly. There were no abnormalities on pulmonary radiography. Biopsy of the ulcerative lesion on his chest showed no bacteria, but spherical and encapsulated blastoconidia. Mycological culture on Sabouraud dextrose agar incubated at 30◦C allowed the growth of typical Cryptococcus colonies after 48 hours. Subculture on agar Canavanine-Glicin-Bromotimol (CGB) confirmed the species as C. neoformans [6]. Other tests to uncover an obscure immunossupression predisposition, showed a non-reactive HIV test and no hematological abnormalities. In addition, blood biochemical tests such as glucose and assays of hepatic and renal status were within the normal parameters. Patient was considered an immunocompetent host and was treated with fluconazole 600 mg BID PO for 6 months. A medical follow-up after 50 days (D50) from the beginning of antifungal therapy (January 2021) showed an improvement of the lesion on the face and the remission of the chest lesion (Fig. 1). He reported pain and an increase of the ulcerative lesion of his right forearm. A second follow-up visit, thirty days later (80 days of treatment) (D80), showed clinical cure of the lesion on the right forearm, however a new lesion on his face (cheek). Because of the new lesions, the treatment with fluconazole (600 mg/day) was maintained for at least 6 months. In the next follow-up, 30 days later (110 days of treatment) (D110), the patient had a great improvement in the cheek lesion, but some local residual activity and a new active lesion in leg, so the treatment and follow-up were continued (Fig. 1). The patient had difficulty adhering to treatment, with self-reported interruptions and a suspicion of self-inflicted local injuries that could not be confirmed.
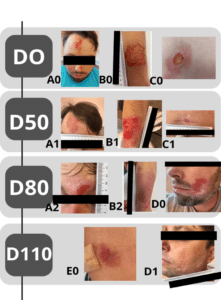
Figure 1: Timeline showing the clinical evolution of the lesions during the follow-up in a patient diagnosed with PCC. D0: First appointment. D50: 50 days of treatment. D80: 80 days of treatment. D110: 110 days of treatment with fluconazole 600 mg/day. A to E: evolution of the patient’s lesions. A0-A2: Forehead lesion. B0-B2. Right arm lesion. C0-C1. Chest lesion. D0-D1: New lesion in the cheek. E0. Leg active lesion on D110.
Discussion
C. neoformans is largely an opportunistic agent, causing disease in immunosuppressed patients, especially in HIV-AIDS, where it is responsible for 15% of all deaths [3,5]. In a local study, cryptococcosis was an HIV/AIDS-defining disease in 40% of cases, so it is important to rule out causes of immunosuppression associated with fungal infection [7]. On the other hand, systemic cryptococcosis in hosts without impairment of immune system is rare and PCC in these immunocompetent patients even more rarely described on the literature [2,8-16]. Our case contributes to the scarce data; we show an immunocompetent patient, without any typical predisposition factor for cryptococcosis, that fulfilled all criteria for PCC diagnoses caused by C. neoformans [1]. A study carried out in Brazil from 2005 to 2010, showed 11 cases of PCC, with only three caused by C. neoformans in immunocompetent patients. In disagreement with our case, antifungal therapy with high dosage fluconazole was effective in others, progressing to complete clinical cure [14]. However, our patient had a history of missing clinical appointments and reported treatment interruption in the 1 year of treatment, which was probably the reason for the persistence of some lesions and appearance of new ones during a long period of observation, despite the correct treatment. Our patient reported continuous exposure to pigeon excrement in his workplace, since a port and refinery environment has large sheds that are a home for many animals, including pigeons. Our hypothesis is that he was infected by traumatic inoculation of the fungus via a contaminated surface, possibly at sites of prior injury. Kronstand, et al., reported that a high fungal load, to which the host is exposed, can explain the disease in immunocompetent persons, via the inhalation of a large number of infectious spores [17]. However, the route of exposure via traumatic inoculation seems more strongly related to PCC [4,16,18-20]. Since the habitat of pigeons and other birds is a reservoir for Cryptococcus species in the environment, we believe this mycosis resulted from an occupational exposure in our case, as has already been described in the literature [21,22]. This expands the perspective of the epidemiology of this fungal infection in immunocompetent persons as well [23].
Conclusion
Our case reported reinforces the importance of a complete investigation for a correct diagnosis, demonstrating the relevance of mycological laboratory exams to making the diagnosis of PCC and enabling start of appropriate therapy, essential to a favorable outcome. Physicians must be aware of these kinds of uncommon fungal infections, even in immunocompetent patients.
Author Contributions
JLB Study design, development, collection and data interpration, diagnostic evaluation, case discussion and writing all. RPB collection and data interpration, case discussion, manuscript revision. VRP study design, development, data interpration, writing sections and manuscript revision. LMS study design, development, data interpration, writing sections and manuscript revision. ABG patient follow-up and case discussion, diagnostic evaluation and therapeutic decisions, collection of data, manuscript revision. LZD patient follow-up and case discussion, diagnostic evaluation and therapeutic decisions, collection of data, manuscript revision. DAS study design, data interpratation, case discussion, writing all, manuscript revision and review of writing in english by native speaker. MOX study design, development, collection and data interpration, diagnostic evaluation, case discussion, writing all and manuscript revision.
Acknowledgment
The authors are grateful to Health Science Post-graduation program, of College of Medicine from Federal University of Rio Grande, to Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Brazil), to the national council Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and the funding agency Fundação de Apoio a Pesquisa do Rio Grande do Sul (FAPERGS; grant 10/2022).
Conflict of Interest
The authors have no conflict of interest to declare.
References
- Noble, R.C, Fajardo, L.F. Primary cutaneous cryptococcosis: Review and morphologic study. Am J Clin Pathol. 1972;57:13-22.
- Revenga F, Paricio JF, Merino FJ, Nebreda T, Ramirez T, Martínez AM. Primary cutaneous cryptococcosis in an immunocompetent host: case report and review of the literature. Dermatol. 2002;204(2):145-9.
- Noguchi H, Matsumoto T, Kimura U, Hiruma M, Kusuhara M, Ihn H. Cutaneous cryptococcosis. Med Mycol J. 2019;60(4):101-7
- Neuville S, Dromer F, Morin O, Dupont B, Ronin O, Lortholary O. French cryptococcosis study group. Primary cutaneous cryptococcosis: a distinct clinical entity. Clin Infect Dis. 2003;36(3):337-47.
- World Health Organization. Guidelines for the diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children. 2018;1-65.
- Min KH, Kwon-Chung KJ. The biochemical basis for the distinction between the two Cryptococcus neoformans varieties with CGB medium. Zentralbl Bakteriol Mikrobiol Hyg A. 1986;261(4):471-80.
- Da Silva LB, Bock D, Klafke GB, Sanchotene KO, Basso RP, Benelli JL, et al. Cryptococcosis in HIV-AIDS patients from Southern Brazil: Still a major problem. J Mycologie Médicale. 2020;30(4):101044.
- Tore O, Akcaglar S, Kazak E, Heper Y, Akalin H, Hakyemez B, et al. Multiple intracranial abscesses due to Cryptococcus neoformans: an unusual clinical feature in an immunocompetent patient and a short review of reported cases. Medical Mycol. 2010;48(2):398-401.
- Day JN, Hoang TN, Duong AV, Hong CT, Diep PT, Campbell JI, et al. Most cases of cryptococcal meningitis in HIV-uninfected patients in Vietnam are due to a distinct amplified fragment length polymorphism-defined cluster of Cryptococcus neoformans var grubii VN1. J Clin Microbiol. 2011;49(2):658-64.
- Fisher JF, Valencia-Rey PA, Davis WB. Pulmonary cryptococcosis in the immunocompetent patient-many questions, some answers. Open Forum Infect Dis. 2016;3(3):167.
- Khattab A, Patruni S, Sealey ML. Rare presentation of cryptococcal meningitis in an immunocompetent patient. BMJ Case Rep. 2019;12(5):e230003.
- Dienstmann G, Avi KT, Leite LA, Alano JS, de Souza ML, da Silva MM, et al. First case report of fulminant septic shock from meningococcemia associated with Cryptococcus neoformans coinfection in an immunocompetent patient. Medical Mycol Case Reports. 2019;26:44-6.
- Chen M., Xu N, Xu J. Cryptococcus neoformans meningitis cases among China’s HIV-infected population may have been severely under-reported. Mycopathologia. 2020;185(6):971-4.
- Marques SA, Bastazini Jr I, Martins AL, Barreto JA, Barbieri D’Elia MP, Lastória JC, et al. Primary cutaneous cryptococcosis in Brazil: report of 11 cases in immunocompetent and immunosuppressed patients. Int J Dermatol. 2012;51(7):780-4.
- Murad A., Murphy A. Primary cutaneous Cryptococcus neoformans serotype D presenting as painful ulcer and nodules on elbow of an immunocompetent patient. Ir J Med Sci. 2014;183(4):691-2.
- Choi H, Kim YI, Na CH, Kim MS, Shin BS. Primary cutaneous cryptococcosis in an older immunocompetent patient: A case report. Ann Geriatr Med Res. 2020;24(2):148-51.
- Kronstad JW, Attarian R, Cadieux B, Choi J, D’souza CA, Griffiths EJ, et al. Expanding fungal pathogenesis: Cryptococcus breaks out of the opportunistic box. Nature Rev Microbiol. 2011;9(3):193-203.
- Christianson JC, Engber WD. Primary cutaneous cryptococcosis in immunocompetent and immunocompromised hosts. Med Mycol. 2003;41(3):177-88.
- Pau M, Lallai C, Aste N, Atzori L. Primary cutaneous cryptococcosis in an immunocompetent host. Mycoses. 2010;53(3):256-8.
- Shalom G, Horev A. Primary cutaneous cryptococcosis: An unusual injection site infection. Case Reports Dermatol. 2020;12(2):138-43.
- Rosario I, Acosta B, Colom F. La paloma y otras aves como reservorio de Cryptococcus spp. Revista Iberoamericana de Micología. 2008;25(1):S13-8.
- Malhotra A, Rao Q, Kelly S, Schwartz D, Chow R. A rare presentation of cryptococcal meningoencephalitis in an immunocompetent individual. Clin Pract. 2017;7(4):1002.
- Enoch DA, Yang H, Aliyu SH, Micallef C. The changing epidemiology of invasive fungal infections. Human fungal pathogen identification: methods and protocols. 2017:17-65.
This work is licensed under a Creative Commons Attribution 2.0 International License.


