Jimmy Tat1, Andrew Marsh2, Richard Jenkinson1,2*
1Department of Surgery, Division of Orthopaedic Surgery, University of Toronto, Toronto, ON, Canada
2Sunnybrook Health Sciences Centre, University of Toronto, Toronto, ON, Canada
*Correspondence author: Richard Jenkinson, Sunnybrook Health Sciences Centre, 2075 Bayview Ave. Toronto, ON, Canada; Email: [email protected]
Published On: 20-03-2023
Copyright© 2023 by Jenkinson R, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: A case series demonstrating the use of a tibia intermedullary nail placed in a retrograde fashion through the calcaneus and talus as a Tibiotalocalcaneal (TTC) arthrodesis salvage technique in three separate patients.
Case Presentation: The first case, an 80-year-old female with a previous Total Knee Arthroplasty (TKA) and ipsilateral open tibia shaft fracture developed a septic non-union with hardware failure. Given her multiple comorbidities, she was treated with a long TTC arthrodesis using a retrograde tibial nail to preserve her soft tissue and encourage earlier mobilisation. The second case, was a 55-year-old male with an open right pilon fracture and multiple surgeries due to non-union of his fracture, including failed TTC with hindfoot nail, he was salvaged with a TTC arthrodesis using a long TTC arthrodesis with a retrograde tibial nail. The last patient, a 30-year-old male who fell 25 feet and suffered a right open pilon fracture required multiple surgeries due to septic non-union, and eventually achieved union after a TTC arthrodesis with osteotomy for deformity correction, both of which were stabilized using a retrograde tibial nail.
Conclusion: In this case series, the patients underwent revision surgery for non-union using a long TTC arthrodesis construct with a retrograde tibial nail ultimately achieving union. We found that for select patients, a retrograde tibial nail for TTC arthrodesis was a useful option to reduce complications, achieve union, and help to encourage early mobilization and return of function.
Keywords: Tibiotalocalcaneal; Arthrodesis; Revision; Intramedullary Nail; Retrograde Nailing
Abbreviations
TTC: Tibiotalocalcaneal; TKA: Total Knee Arthroplasty; AOFAS: American Orthopedic Foot and Ankle Society
Introduction
Tibiotalocalcaneal (TTC) arthrodesis is used in the treatment of severe end-stage arthritis of the ankle and subtalar joint. It is also a helpful salvage procedure in severe acute trauma, failed previous operations, and severe malalignment deformities. Different surgical techniques are used to achieve arthrodesis including intramedullary nailing, plate and screw constructs, external fixation, and cast immobilization [1-3]. Retrograde TTC intramedullary hindfoot nails are frequently used for being minimally invasive and is thought to provide superior biomechanical properties with higher bending stiffness, increased rotational stability, and dynamic compression capability (compared with plate and screw constructs) [4-6].
To our knowledge this is the first study to describe the retrograde insertion of a tibial nail to achieve a TTC arthrodesis. There have been previous variations of a tibia nail specifically designed for retrograde insertion. Kuhn developed a small-caliber prototype retrograde tibial nail implant, which was introduced through a 2-cm-long incision at the tip of the medial malleolus in a cadaver model with a distal tibia fracture [7]. Another previous retrograde tibial nail design was developed and used in patients with very proximal tibial fractures or osteotomies. This device spanned only the tibia shaft and did not cross the ankle joint [8]. We introduce the use of a retrograde tibia nail that is not unlike the original TTC nails that used antegrade femoral nails in a retrograde manner (prior to creation of hindfoot nails) [9-10]. We propose that the tibial nail provides some advantages over the femoral nail. The femoral nail has less inherent angulation. A femoral nail made for a piriformis start point is straight and cannot provide the valgus-orientation preferred in a hindfoot nails. While a greater trochanter start point femoral nail may provide some angulation, it will have a proximal to distal AP bow in the shaft that may not accommodate a tibia shaft. The femoral nail also provides less options for distal screw fixation at the ankle, given the nail’s proximal lag screws utilize two parallel screws in one plane. As such, we think the tibia nail provides a better alternative to accommodate the distal tibia and hindfoot, since it allows for more options for distal fixation at the ankle into both the talus and calcaneus in orthogonal planes.
This study presents 3 cases using a retrograde tibiotalocalcaneal nail with an off-label use of tibial intermedullary nail as a salvage technique. In the first case, we describe a technique for intramedullary nailing of tibial fractures below a Total Knee Arthroplasty (TKA) using a retrograde tibial nail to preserve the tibial prosthesis component. The subsequent two cases demonstrate a failed hindfoot fusion due to non-union and patients requiring revision TTC arthrodesis with a retrograde tibial nail.
Case Presentation
Case 1
An 80-year-old female with a previous Total Knee Arthroplasty (TKA) suffered an ipsilateral periprosthetic open tibia shaft fracture that was complicated by septic non-union, and underwent fracture stabilization using a retrograde tibial nail and TTC arthrodesis.
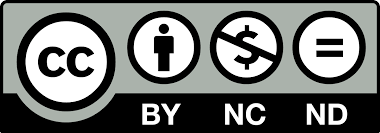
The patient had a past medical history of hypertension, overactive bladder, peripheral vascular disease, and atrial fibrillation on clopidogrel. She underwent an ipsilateral TKA in 2012 which was functioning well. Unfortunately, she presented to our trauma center after being struck by a transport truck while crossing the street in 2019. She suffered a left open segmental tibia-fibula shaft fracture (Gustilo 3A) with a large medial mid-tibial wound, left open bimallolar ankle fracture, and multiple left foot fractures (navicular, calcaneous fracture, medial and lateral cuneiforms, impaction of dorsal cuboid, metatarsal digits 1-4) (Fig. 1).
Her tibia fracture was distal to her TKA, and given there was no evidence of implant loosening or periprosthetic fracture, she underwent irrigation and debridement and open reduction internal fixation of her tibia. An 18-hole, 4.5 mm proximal locking anterolateral plate was utilized for fixation due to her ipsilateral left TKA. For the fibula, a distal fibular locking plate with 2.7 mm and 3.5 mm screws and 2 syndesmosis screws through the plate (Fig. 2). Primary closure of her open tibia wound was achieved. She was discharged from the hospital with ongoing wound care. However, she returned later due to persistent wound healing issues.
Her outpatient follow-up occurred during the COVID-19 pandemic and she was only seen in a virtual clinic by telephone assessments for the first 7 months. Unfortunately, this delayed her diagnosis of a septic non-union. At her 8 month in-person visit, her wound had developed a 1-2 cm sinus tract overlying the medial distal tibia wound with purulent drainage. Radiographs demonstrated a non-union of her tibia segmental midshaft fracture and wound cultures grew polymicrobial organisms (E. Coli, MSSA, and Group B streptococcus). A course of antibiotics, guided by our infectious disease team, was trialed. However, she unfortunately did not improve. At 10 months, she represented to our hospital emergency department with a broken plate and was admitted for revision surgery (Fig. 3).
We recommended proceeding with an intermedullary fixation using an unconventional approach with a retrograde tibial nail to create a tibiotalocalcaneal arthrodesis and span the tibia shaft non-union site. This was proposed due the patient’s low functional demands, poor health status, compromised soft tissue envelope, and peripheral vascular disease. We had a thorough discussion of surgical management options with the patient and family obtaining informed consent for this surgical plan.
The operative procedure involved removal of the hardware, irrigation and debridement at the septic non-union site, followed by a retrograde tibiotalocalcaneal nail. A tibial nail (Trigen Meta Nail 11.5 mm x 320 mm, Smith and Nephew, Inc, Memphis, TN) was placed in a retrograde direction at the calcaneus with the Herzog curve providing a laterally directed valgus bow and resulted in 10 degrees valgus alignment across the hindfoot and ankle. This is similar to specifically designed hindfoot nails (Table 1). Postoperatively, she was kept non-weight bearing and placed on long term antibiotics. She was seen in clinic at 4 weeks and weightbearing was initiated. Her radiographs demonstrated ongoing callus formation at the previous non-union site. At 6 months, she continued to see improvements in her mobility and pain. She was no longer requiring antibiotics and had bridging callus at her non-union site.
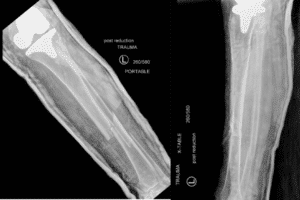
Figure 1: Case 1: Radiographs of left tib-fib showing left tibia open segmental tibia-fibula shaft fracture (Gustilo 3A) with a large medial mid-tibia wound and a left open bimallolar ankle fracture.

Figure 2: Case 1: Radiograph of left tib-fib. The TKA periprosthetic fracture was fixed using an 18 hole, 4.5mm proximal locking anterolateral plate due to her ipsilateral left TKA. For the fibula, a distal fibular locking plate with 2.7 mm and 3.5 mm screws and 2 syndesmosis screws through the plate.
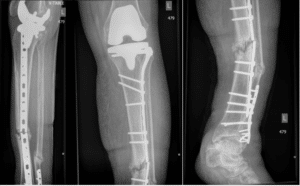
Figure 3: Case 1: Radiographs showing left tib-fib. At 10 months, she represented to our hospital emergency department with a broken the plate and a diagnosis of septic non-union of her tibia segmental midshaft fracture.

Figure 4: Case 1: Post operative X-rays of left tib-fib and ipsilateral TKA showing a retrograde tibiotalocalcaneal. The tibial nail (Trigen Meta Nail 11.5mm x 320 mm, Smith and Nephew, Inc, Memphis, TN) was placed the Herzog curve providing a lateral directed position and a 10 degrees valgus alignment across the hindfoot and ankle.
Nail (Manufacturer) | Valgus | Length (mm) | Width (mm) | Distal Screw Options |
Phoneix Ankle Arthrodesis Nail (Biomet, Warsaw, IN) | Straight | 150 180 210 240 270 300 | 10 11 12 | One transverse talus, one transverse calcaneus, and one PA calcaneus. Jig allows another screw bypassing the nail |
Panta (Integra, Plainsboro, NJ) | Straight
| 150 180 210 240 | 10 11 12 13 | One transverse talus and two PA calcaneus |
T2 (Stryker, Kalamazoo, MI) | 5 deg | 150 200 300 | 10 11 12 | One transverse talus, one transverse calcaneus, and one PA calcaneus |
Hindfoot Fusion Nail (Synthes, West Chester, PA) | 10 deg | 150 180 240 | 10 11 12 | One PA talus, two PA calcaneus. (One of these PA screws can be a large spiral screw) |
Trigen Hindfoot Fusion Nail (HFN) (Smith and Nephew, Memphis, TN) | Straight
| 160 200 250 320 340 360 | 10 11.5 | One transverse talus, one PA calcaneus, and one oblique PA calcaneus to talus |
Versanail (DePuy, Warsaw, IN) | Straight | 150 200 250 300 | 10 12 | One transverse talus and two transverse calcaneus, or one PA talus and two PA calcaneus |
Valor Hindfoot Fusion System (Wright Medical Technology, Memphis, TN) | Straight | 150 200 250 300 | 10 11.5 | One transverse talus, one PA calcaneus, and one oblique PA calcaneus to talus |
Table 1: Hindfoot Intramedullary Nail Design Options (Adapted from Thomas 2012).
Case 2
A 55-year-old male healthy, non-smoker was in a motor vehicle accident in 2017 and suffered bilateral ankle injuries including an open right pilon fracture and a closed left ankle bimalleolar ankle fracture. His right ankle was unfortunately complicated by septic non-union, and he underwent a revision TTC arthrodesis with a retrograde tibia intermedullary nail.
The patient’s right ankle was initially managed at another hospital with irrigation and debridement of the anterior ankle wound with stabilization using a spanning ankle external fixator (Fig. 4-6). He was then transferred to our institution for definitive fixation. He was treated with open reduction and internal fixation. 10 mL of OsteoSet T pellets impregnated with Tobramycin were used to help fill the meta-diaphyseal bone defect. Unfortunately, he went on to have a septic non-union in his distal tibia. He failed multiple courses of antibiotics with revision surgeries to treat his non-union. We followed him in clinic for the next eight months, and there was no progression in fracture healing and he had persistent ankle pain. The hardware was subsequently revised to a single dynamic compression plate over the medial distal tibia (Fig. 7). However, the non-union persisted. After another eight months he was revised to a TTC hindfoot nail (13 x 240 mm synthesis expert hind foot nail) (Fig. 8). He returned 7 months later with a draining sinus in the anterior ankle wound with positive cultures that grew Beta hemolytic streptoccoccus group G. A staged procedure was then undertaken. In the first stage, we removed all hardware and treated with 6 weeks of IV antibiotics, followed by another 6 weeks of oral antibiotics (Fig. 9). In stage 2 of his treatment, the infection had been eradicated and he underwent revision TTC using a standard tibia nail (Smith and Nephew, 13 mm x 320 mm) placed retrograde. Iliac crest autograft was used at the arthrodesis site to encourage union (Fig. 9).
Post-operatively he was initially touching weight bearing for the first 12 weeks, at which time he was transitioned to weight bearing as tolerated. At 6 months, he returned to walking with no pain in the ankle or distal tibia. He had no further wound healing issues or drainage. His only complaint was a mild discomfort in the plantar aspect of his heel, near incision of the nail insertion. Radiographs demonstrated a well fused TTC arthrodesis.
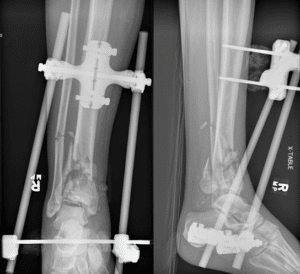
Figure 5: Case 2: Radiograph of right ankle showing an open right pilon fracture status post stabilization using a spanning ankle external fixator (Fig. 5).

Figure 6: Case 2: Radiograph of right ankle. Fixation of the right pilon fracture with a 6-hole dynamic compression plate for the fibula fracture, and for the distal tibia we used several periarticular anterior-to-posterior 2.4 screws, as well as an anteromedial low profile Synthes locking plate and smaller anterior T-plate 3.5 mm distal tibia locking plate.
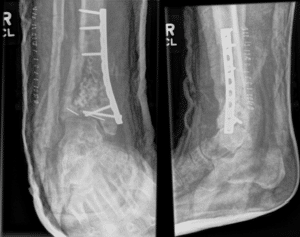
Figure 7: Case 2: Radiograph of right ankle after removal of ankle hardware and revision fixation to a single dynamic compression plate over the medial distal tibia (Fig. 7).
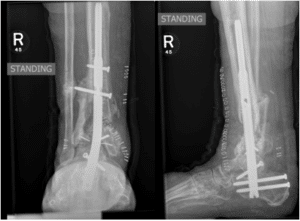
Figure 8: Case 2: Radiograph of right ankle. After eight months of failed treatment of non-union we performed a TTC arthrodesis using a hindfoot nail (13 x 240 mm synthes expert hindfoot nail).

Figure 9: Case 2: Staged procedure for septic non-union of previous TTC hindfoot nail. First stage involved all hardware with radiographs of the left ankle A) AP view, B) lateral view. The second stage involved the revision TTC nail using as retrograde tibial nail and iliac crest autograft shown in radiographs of left ankle, C) AP view and D) lateral view.
Case 3
A 30-year-old healthy male fell from a height of 25 feet in 2013 and suffered bilateral ankle injuries which were similar to Case 2. Orthopaedic injuries included a right open pilon fracture and left closed bimalleolar ankle fracture (Fig. 10). He underwent multiple revisions surgeries due to non-union and eventually achieved union after a revision TTC arthrodesis with a retrograde tibia intermedullary nail.
His right open pilon fracture was first managed at another hospital with acute irrigation and debridement and fracture fixation. The fibula fracture was fixed with a 6-hole dynamic compression plate and the distal tibia with a medial low profile distal tibia locking plate (Fig. 10). This was done through a direct lateral incision over the fibula and anteromedial tibial incision. Unfortunately, after 5 weeks, the medial plate (which was subcutaneous) had broken through the medial soft tissue creating a skin defect and exposed plate and bone. He was transferred to our institution for care.
He underwent a total of 6 surgeries between 2013 and 2017. He was initially treated in a staged manner with plans to treat him definitively using a TTC arthrodesis with a hindfoot nail after infection eradication and soft-tissue stability. All implants were removed followed by irrigation and debridement, antibiotic beads were placed and the fractures were provisionally stabilized using a spanning external fixator (Fig. 11). His wounds were closed primarily. He was placed on long term IV antibiotics post-operatively. At 8 weeks, we removed the external fixator and he was placed in a circumferential below knee cast. At this time, radiographs showed a non-union at the distal tibia with a large bone defect in the diaphyseal region, but otherwise adequate alignment. His soft tissue defect healed without any complication. After 4 months, the patient back to the operating room for right ankle TTC arthrodesis with iliac crest bone graft. A hindfoot nail (13 mm x 240 mm nail synthes hindfoot nail) was utilized for stabilization (Fig. 12).
At 11 months, a repeat CT scan of his right ankle showed a persistent atrophic non-union of the distal tibia with fused ankle and subtalar joints. There were no signs or symptoms of infection, therefore a revision with longer nail construct was implemented. A revision TTC arthrodesis using retrograde tibial nail (13 mm x 400 mm length tibial TriGen nail) was implanted (Fig. 13). The tibia was over-reamed to size 14.5 and the angle the Herzog curve of the tibial nail was placed to match the previous TTC valgus position. Postoperatively, partial weight bearing with a fracture boot at 2 weeks was permitted and full weight bearing at 6 weeks. At 2 months post operatively, the patient was weight bearing with no ankle pain, and radiographs demonstrated healing of the non-union site. His only complaint was stiffness and a leg length discrepancy of 1.4 cm (which he was adequately managed with a shoe lift).
Approximately one year later, he returned with new pain and swelling over the anterior proximal leg near the proximal AP locking screw. Though there was no frank drainage, there was concern of infection given he had elevated inflammatory markers (CRP 138, ESR 15) and new pain. He was subsequently taken to the OR for removal of hardware and irrigation and debridement with insertion of OsteoSet T pellets with antibiotics. Intraoperative cultures grew Coagulase Negative Staphylococcus (CNST) and he was treated with 6 weeks of IV vancomycin. Nine months later he returned to our clinic and unfortunately suffered a new fracture through his previous distal tibia non-union site from an accident (Fig. 14). He had an accident where he had to put forceful weight through his tibia associated with a motor vehicle collision. The plan was to treat him with a similar revision TTC arthrodesis using a retrograde tibial nail, however he was lost to follow up for 4 months. When he returned, his x-rays demonstrated progressive healing of the fracture non-union site (though malunited) and it was decided to continue with nonoperative management (Fig. 14).
Unfortunately, he remained symptomatic with persistent varus bowing deformity in distal tibia. A repeat CT showed a malunion of the right tibia and internal rotation in varus deformity and his repeat inflammatory markers did not suggest infection (CRP 3, ESR 1). At twelve months after his re-injury, a supramalleolar double osteotomy and distal fibula osteotomy of the right ankle was performed to correct the varus and internal rotation. A tibia nail (13 mm x 400 mm, TriGen Smith and Nephew) was inserted as a retrograde nail for TTC arthrodesis. The tibia was over-reamed to 15 mm to allow for insertion of the 13 mm nail (Fig. 15). He did well postoperative, his pain improved and he was ambulating with a stable ankle. Radiographs at 6 months post-op showed osseous bridging posterior at the osteotomy site and ongoing healing in the anterior osteotomy, and a fully fused subtalar and tibiotalar joint. At 2 years post op his osteotomy demonstrated complete union.

Figure 10: Case 3: Radiograph of right tib-fib showing a right open pilon fracture.

Figure 11: Case 3: Radiograph of right ankle. Initial management of the right pilon ankle fracture with irrigation and debridement, antibiotic beads, IV antibiotics and spanning ankle external fixator.

Figure 12: Case 3: Right ankle TTC arthrodesis with iliac crest bone graft. We used a hindfoot nail (13 mm x 240 mm nail synthes hindfoot nail), and reamed to size 14.

Figure 13: Case 3: Radiograph of right tib-fib showing revision TTC arthrodesis using a retrograde tibial nail (13 mm x 400 mm length tibial TriGen nail).
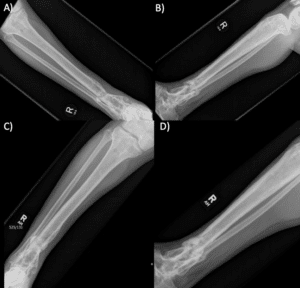
Figure 14: Case 3: The patient suffered a new fracture through his previous distal tibia non-union site shown in the radiograph of his right tib-fib, A) AP view B) lateral view. He was lost to follow up and represented 4 months lateral. Repeat X-rays of his tib-fib showed progressive healing of the fracture non-union site, C) AP view, D) lateral view.

Figure 15: Case 3: The patient’s right tibia malunion (internal rotation in varus deformity) was managed with a supramalleolar double osteotomy of the right tibia to correct the varus and internal rotation, and an osteotomy of the distal fibula. The osteotomy was then stabilized with a retrograde tibia nail (13 mm x 400 mm, TriGen Smith and Nephew) TTC arthrodesis.
Discussion
With this case series we present a creative surgical technique using a retrograde tibial intermedullary nail to perform a tibiotalocalceneal arthrodesis as a salvage technique in challenging cases. We demonstrate that retrograde tibial nails can be useful in achieving union in complex trauma cases where conventional hindfoot TTC nails have been unsuccessful. The added length of a conventional antegrade tibial nail can provide stability when conventional TTC nails are not of adequate length. The Herzog curve of antegrade tibial nails can be modified to allow for appropriate valgus alignment of the hindfoot when using these implants. We also demonstrated a unique circumstance in which a retrograde tibia nail was used in a periprosthetic TKA fracture with previous failed internal fixation of the tibial shaft. In this patient, there were special considerations due to her medical comorbidities including peripheral vascular disease and a poor soft tissue envelope in a low demand patient.
Our surgical technique consisted of using the instruments available in a standard set of antegrade tibial intermedullary nail. We used the Trigen MetaNail (Smith and Nephew, Inc, Memphis, TN) with varying dimensions (diameter 11.5 to 13 mm; length 320 to 400 mm). The patients were placed supine. We used the starter wire, and inserted it through the calcaneus up into the talus using fluoroscopy in AP and lateral views. We placed the tibial nail with the Herzog curve providing a lateral directed position and a 10 degrees valgus alignment across the hindfoot and ankle. This is similar to specifically designed hindfoot nails. The joint surfaces were not routinely prepared. The guidewire was then passed, followed by the opening reamer. We typically sequentially reamed for a total of 1 mm above the diameter of the nail, and in revision cases we reamed 1.5 mm above the previous nail diameter. The nails were locked distally by applying the targeting arm and placing 2 distal locking screws through the calcaneus and the talus with a lateral-to-medial transverse orientation. This is unlike most current hindfoot systems which provide both a posterior-to-anterior distal screw into the calcaneus and a lateral-to-medial screw into the talus; with the thought that the combination of screws increases rotational stability [11-12]. We found that these two transverse screws, cross pinned into the calcaneus and talus and were able to secure the distal aspect of the nail. Rotation was confirmed and the nail construct was impacted before proximal locking from anterior to posterior. Proximal locking was done with standard freehand technique using fluoroscopy. The patients were kept touch weight-bearing for a minimum of 2-6 weeks until soft tissue healing was satisfactory.
The ideal position for the hindfoot with TTC arthrodesis is described to be 5 degrees of valgus, 5-10 degrees external rotation (compared to the contralateral limb), and a neutral position in the sagittal plane for dorsiflexion and plantar flexion [13-14]. This can be achieved by maintaining the correct ankle position when preparing the nail such as while drilling the Kirschner wire and reaming the canal. Modern hindfoot nails are designed with 5-10 degrees of a valgus curve in the distal nail to further help attain this hindfoot alignment [1]. The design of a standard tibial antegrade nail also has a Herzog bend of 10 degrees that can be used to build in 10 degrees of valgus (laterally directed position and avoids varus) alignment in the hindfoot and ankle when placed in a retrograde fashion. There is some evidence in TTC arthrodesis that maintains the patient’s physiological valgus hindfoot angle can have improve clinical outcomes and offers the theoretical advantage of less dysfunction and arthritis in adjacent joints [13]. The tibia nail provides a good alternative to accommodate the distal tibia and hindfoot, since there are a number of options for distal fixation at the ankle that can be placed into both the talus and calcaneus in orthogonal planes (Table 2).
The use of retrograde tibia nail provides an option for long TTC nail that may not be regularly available. The standard TTC arthrodesis hindfoot nail is 150 mm to 200 mm long, with a maximum of 300-360 mm depending on the manufacturer (these larger sizes often require advance requests for access) (Table 1); compared to tibia nails which can allow for a nail length of 160 mm to 500 mm (Table 1). There are advantages to having a longer device that ends in the proximal tibial metaphysis, rather than distal to middle tibia. A longer device can improve load sharing across the tibia and decrease strain at the distal tibia near the arthrodesis site. Additionally, a long intramedullary device has also been shown to decrease stress concentration at the proximal junction of the nail-tibia composite and decrease the risk of fracture [9,15-16]. Though periprosthetic fractures in TTC nails are a rare complication, it may be important in osteopenic patients. For instance, in revision salvage procedures patients have been non-weight-bearing for long periods of time and likely suffer from disuse osteopenia that may increase their risk of fracture [16]. In our case series, we also showed a unique circumstance in our patient with a periprosthetic TKA tibia shaft fracture, where a longer TTC nail was necessary to appropriately span the midshaft tibia fracture (and a traditional hindfoot nail would have been too short to stabilize the fracture).
Non-union in TTC arthrodesis is a frequent complication that often necessities revision surgery. However, there remains to be a clear technique to best address this complication. Previous methods to minimize the risk of non-union include using systems with internal compression at the arthrodesis site [11]. It is thought that compression can promote stability and bone-healing at the arthrodesis site [18]. However, this is an area of ongoing controversy. In a retrospective review of 198 patients with TTC hindfoot nails, there was statistically no difference in union rate with and without internal compression [18,19]. Nonetheless, traditional hindfoot nails have the option for internal compression built-in. There are also new implants specifically designed to create compression using a pseudoelastic intramedullary nail system or a blade plate construct [11,17]. The use of tibia nail may also be an option of using dynamic compression for the surgeon. This can be done with using the oblong hole when locking into the with tibia shaft for axial compression.
There were several limitations to this study. This was as small case study of only 3 patients due to the narrow indications we found to use a retrograde tibial nail, nonetheless, we demonstrated that it is a useful salvage option. The patients had limited follow-up and outcome measures. Our follow-up ranged from 6-months to 2-years and we were not able to further characterize the patients outcomes with clinical scores (e.g. AOFAS score) due to the retrospective nature of the case report. Lastly, we do not routinely denude the articular surfaces of the tibiotalar and subtalar joint during TTC arthrodesis. Preparing the tibiotalar and subtalar joints is an area of controversy and this could affect our arthrodesis results [20]. However, did have good clinical and radiographic evidence of successful union of the tibiotalar and subtalar in our patient series.
Conclusion
We have demonstrated that the use of a retrograde tibial nail for TTC arthrodesis as a salvage technique for tibial shaft fractures is feasible and effective. This technique was useful in achieving union in complex trauma cases where conventional hindfoot TTC nails had previously failed to heal the distal tibia fractures. We also demonstrated a unique circumstance in which a retrograde tibial nail was used in stabilization of a periprosthetic TKA tibial shaft fracture. For select patients, the treatment of tibial shaft fractures with retrograde tibial nail as a TTC construct can help to reduce complications in comparison to traditional management strategies and encourage earlier mobilisation and return of function.
Conflict of Interest
The authors have no conflict of interest to declare.
References
- Thomas RL, Sathe V, Habib SI. The use of intramedullary nails in tibiotalocalcaneal arthrodesis. JAAOS. 2012;20(1):1-7.
- Maurer RC, Cimino WR, Cox CV, Satow GK. Transarticular cross-screw fixation. A technique of ankle arthrodesis. Clin Ortho Rel Res. 1991;(268):56-64.
- Mears DC, Gordon RG, Kann SE, Kann JN. Ankle arthrodesis with an anterior tension plate. Clin Orthopaedics and Related Res. 1991;268:70-7.
- Alfahd U, Roth SE, Stephen D, Whyne CM. Biomechanical comparison of intramedullary nail and blade plate fixation for tibiotalocalcaneal arthrodesis. J Orthopaedic Trauma. 2005;19(10):703-8.
- Chiodo CP, Acevedo JI, Sammarco VJ, Parks BG, Boucher HR, Myerson MS, et al. Intramedullary rod fixation compared with blade-plate-and-screw fixation for tibiotalocalcaneal arthrodesis: a biomechanical investigation. JBJS. 2003;85(12):2425-8.
- Bennett GL, Cameron B, Njus G, Saunders M, Kay DB. Tibiotalocalcaneal arthrodesis: a biomechanical assessment of stability. Foot Ankle Int. 2005;26(7):530-6.
- Kuhn S, Appelmann P, Mehler D, Pairon P, Rommens PM. Retrograde Tibial Nailing: a minimally invasive and biomechanically superior alternative to angle-stable plate osteosynthesis in distal tibia fractures. J Orthopaedic Surg Res. 2014;9(1):1-8.
- Hofmann GO, Gonschorek O, Buhler M, Buhren V. Retrograde tibial nailing. Trauma und Berufskrankheit. 2001;3(6):S303-8.
- Woods JB, Shinabarger AB, Burns PR. Periprosthetic fracture after femoral intramedullary nail use in two cases of tibiotalocalcaneal arthrodesis. J Foot and Ankle Surg. 2012;51(2):266-9.
- Goebel M, Gerdesmeyer L, Mückley T, Schmitt-Sody M, Diehl P, Stienstra J, et al. Retrograde intramedullary nailing in tibiotalocalcaneal arthrodesis: a short-term, prospective study. J Foot and Ankle Surg. 2006;45(2):98-106.
- DiDomenico LA, Groner TW. Intramedullary nail fixation for tibiotalocalcaneal arthrodesis. InSpecial Procedures in Foot and Ankle Surg. 2013;153-71.
- Means KR, Parks BG, Nguyen A, Schon LC. Intramedullary nail fixation with posterior-to-anterior compared to transverse distal screw placement for tibiotalocalcaneal arthrodesis: a biomechanical investigation. Foot and Ankle Int. 2006;27(12):1137-42.
- Fang Z, Claaßen L, Windhagen H, Daniilidis K, Stukenborg‐Colsman C, Waizy H. Tibiotalocalcaneal arthrodesis using a retrograde intramedullary nail with a valgus curve. Orthopaedic Surg. 2015;7(2):125-31.
- Hammett R, Hepple S, Forster B, Winson I. Tibiotalocalcaneal (hindfoot) arthrodesis by retrograde intramedullary nailing using a curved locking nail. The results of 52 procedures. Foot and Ankle Int. 2005;26(10):810-5.
- Baker G, Mayne AI, Andrews C. Fixation of unstable ankle fractures using a long hindfoot nail. Injury. 2018;49(11):2083-6.
- Noonan T, Pinzur M, Paxinos O, Havey R, Patwardhin A. Tibiotalocalcaneal arthrodesis with a retrograde intramedullary nail: a biomechanical analysis of the effect of nail length. Foot and Ankle Int. 2005;26(4):304-8.
- Latt LD, Smith KE, Dupont KM. Revision tibiotalocalcaneal arthrodesis with a pseudoelastic intramedullary nail: a case study. Foot and Ankle Specialist. 2017;10(1):75-81.
- Scranton PE Jr. Use of internal compression in arthrodesis of the ankle. J Bone Joint Surg Am. 1985;67:550-5.
- Taylor J, Lucas DE, Riley A, Simpson GA, Philbin TM. Tibiotalocalcaneal arthrodesis nails: a comparison of nails with and without internal compression. Foot Ankle Int. 2016;37(3):294-9.
- Barg A, Saltzman CL. Re: Is subtalar joint cartilage resection necessary for tibiotalocalcaneal arthrodesis via intramedullary nail? a multicenter evaluation. J Foot Ankle Surg. 2017;56(2):413-4.
Article Type
Case Report
Publication History
Received On: 21-02-2023
Accepted On: 13-03-2023
Published On: 20-03-2023
Copyright© 2023 by Jenkinson R, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Jenkinson R, et al. Retrograde Tibia Intramedullary Nailing in Tibiotalocalcaneal Arthrodesis. J Surg Res Prac. 2023;4(1):1-14.
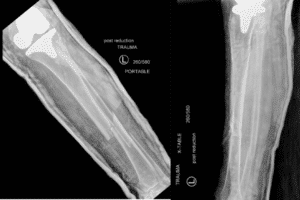
Figure 1: Case 1: Radiographs of left tib-fib showing left tibia open segmental tibia-fibula shaft fracture (Gustilo 3A) with a large medial mid-tibia wound and a left open bimallolar ankle fracture.

Figure 2: Case 1: Radiograph of left tib-fib. The TKA periprosthetic fracture was fixed using an 18 hole, 4.5mm proximal locking anterolateral plate due to her ipsilateral left TKA. For the fibula, a distal fibular locking plate with 2.7 mm and 3.5 mm screws and 2 syndesmosis screws through the plate.
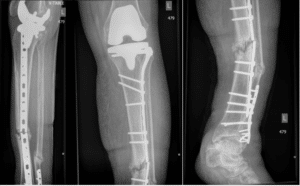
Figure 3: Case 1: Radiographs showing left tib-fib. At 10 months, she represented to our hospital emergency department with a broken the plate and a diagnosis of septic non-union of her tibia segmental midshaft fracture.

Figure 4: Case 1: Post operative X-rays of left tib-fib and ipsilateral TKA showing a retrograde tibiotalocalcaneal. The tibial nail (Trigen Meta Nail 11.5mm x 320 mm, Smith and Nephew, Inc, Memphis, TN) was placed the Herzog curve providing a lateral directed position and a 10 degrees valgus alignment across the hindfoot and ankle.
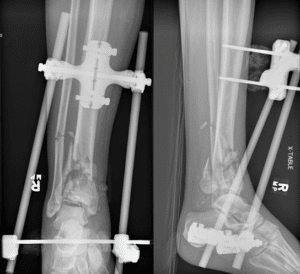
Figure 5: Case 2: Radiograph of right ankle showing an open right pilon fracture status post stabilization using a spanning ankle external fixator (Fig. 5).

Figure 6: Case 2: Radiograph of right ankle. Fixation of the right pilon fracture with a 6-hole dynamic compression plate for the fibula fracture, and for the distal tibia we used several periarticular anterior-to-posterior 2.4 screws, as well as an anteromedial low profile Synthes locking plate and smaller anterior T-plate 3.5 mm distal tibia locking plate.
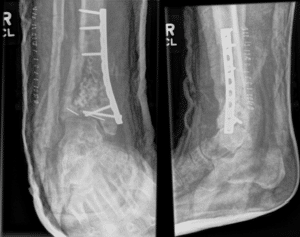
Figure 7: Case 2: Radiograph of right ankle after removal of ankle hardware and revision fixation to a single dynamic compression plate over the medial distal tibia (Fig. 7).
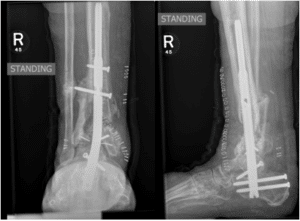
Figure 8: Case 2: Radiograph of right ankle. After eight months of failed treatment of non-union we performed a TTC arthrodesis using a hindfoot nail (13 x 240 mm synthes expert hindfoot nail).

Figure 9: Case 2: Staged procedure for septic non-union of previous TTC hindfoot nail. First stage involved all hardware with radiographs of the left ankle A) AP view, B) lateral view. The second stage involved the revision TTC nail using as retrograde tibial nail and iliac crest autograft shown in radiographs of left ankle, C) AP view and D) lateral view.

Figure 10: Case 3: Radiograph of right tib-fib showing a right open pilon fracture.

Figure 11: Case 3: Radiograph of right ankle. Initial management of the right pilon ankle fracture with irrigation and debridement, antibiotic beads, IV antibiotics and spanning ankle external fixator.

Figure 12: Case 3: Right ankle TTC arthrodesis with iliac crest bone graft. We used a hindfoot nail (13 mm x 240 mm nail synthes hindfoot nail), and reamed to size 14.

Figure 13: Case 3: Radiograph of right tib-fib showing revision TTC arthrodesis using a retrograde tibial nail (13 mm x 400 mm length tibial TriGen nail).
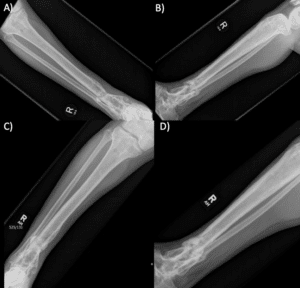
Figure 14: Case 3: The patient suffered a new fracture through his previous distal tibia non-union site shown in the radiograph of his right tib-fib, A) AP view B) lateral view. He was lost to follow up and represented 4 months lateral. Repeat X-rays of his tib-fib showed progressive healing of the fracture non-union site, C) AP view, D) lateral view.

Figure 15: Case 3: The patient’s right tibia malunion (internal rotation in varus deformity) was managed with a supramalleolar double osteotomy of the right tibia to correct the varus and internal rotation, and an osteotomy of the distal fibula. The osteotomy was then stabilized with a retrograde tibia nail (13 mm x 400 mm, TriGen Smith and Nephew) TTC arthrodesis.
Nail (Manufacturer) | Valgus | Length (mm) | Width (mm) | Distal Screw Options |
Phoneix Ankle Arthrodesis Nail (Biomet, Warsaw, IN) | Straight | 150 180 210 240 270 300 | 10 11 12 | One transverse talus, one transverse calcaneus, and one PA calcaneus. Jig allows another screw bypassing the nail |
Panta (Integra, Plainsboro, NJ) | Straight
| 150 180 210 240 | 10 11 12 13 | One transverse talus and two PA calcaneus |
T2 (Stryker, Kalamazoo, MI) | 5 deg | 150 200 300 | 10 11 12 | One transverse talus, one transverse calcaneus, and one PA calcaneus |
Hindfoot Fusion Nail (Synthes, West Chester, PA) | 10 deg | 150 180 240 | 10 11 12 | One PA talus, two PA calcaneus. (One of these PA screws can be a large spiral screw) |
Trigen Hindfoot Fusion Nail (HFN) (Smith and Nephew, Memphis, TN) | Straight
| 160 200 250 320 340 360 | 10 11.5 | One transverse talus, one PA calcaneus, and one oblique PA calcaneus to talus |
Versanail (DePuy, Warsaw, IN) | Straight | 150 200 250 300 | 10 12 | One transverse talus and two transverse calcaneus, or one PA talus and two PA calcaneus |
Valor Hindfoot Fusion System (Wright Medical Technology, Memphis, TN) | Straight | 150 200 250 300 | 10 11.5 | One transverse talus, one PA calcaneus, and one oblique PA calcaneus to talus |
Table 1: Hindfoot Intramedullary Nail Design Options (Adapted from Thomas 2012).