Naiza Monono¹*, Mekone Nkwele², Joshua Tambe¹, Kamo Doka³, Kate-Kan⁴, Mulango Ene¹, Verla Vincent¹
1Department of Internal Medicine and Paediatrics, Faculty of Health Sciences, University of Buea, Cameroon
²Department of Paediatrics, Faculty of Medicine and Biomedical Science, University of Yaounde 1, Cameroon
³Department of Paediatrics, Faculty of Medicine and Biomedical Science, University of Ngoundere, Cameroon
⁴Department of Clinical Science, Faculty of Health Sciences, University of Bamenda, Cameroon
*Correspondence author: Naiza Monono, Department of Internal Medicine and Paediatrics, Faculty of Health Sciences, University of Buea, Cameroon; Email: docnaiza@gmail.com
Published Date: 22-04-2024
Copyright© 2024 by Monono N, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: This practice of scarifying children for medical reasons is common in several African communities with its origin lost in antiquity. A few reasons prompt people to get their children scarified and the practice may have fatal outcomes. In Cameroon where no study has been carried out on this aspect, we saw it necessary to review this practice and its outcome.
Objectives: To assess the prevalence, predisposing factors and outcome of scarification among children less than 15 years old in three hospital settings of the Limbe Health District.
Methods: A three-month hospital based cross-sectional study was carried out. A structured questionnaire was used to collect data from each participant. Data was analyzed using SPSS version 26 and statistical significance was set at p-value <0.05 at 95% confidence interval.
Results: Out of 240 participants enrolled in the study males were predominant (59.6%). We had a scarification prevalence of 57.1% with majority scarified before 5years of age. The majority had fever 96.25%, 41.3% had palpitations and 27.9% had left abdominal pain prompting the act. About 69.3% of the participants were scarified below the left nipple, 75.9% had mechanical scars and 98.5% were performed by a herbalist under unsterile conditions.
Factors prompting scarification were, left abdominal pain, palpitations, having a scarified sibling. While a lower level of education, low-income levels of the carers and generalized body weakness discouraged the act. Among the complications, 0.7% had HIV infection related to the act, 2.2% had infected wounds at the site of the scar and 1.5% death cases were recorded.
Conclusion: In this study, approximately 6 out of 10 children undergo physical insult to treat a reactional hepatomegaly and splenomegaly by a herbalist under unsterile conditions yet, 1 out of 10 of these children died and 3 out of 10 suffered from complications of the act.
Keywords: Children; Splenomegaly; Hepatomegaly; Cameroon
Introduction
Scarification is the practice of incising the skin with a sharp instrument (such as a knife, broken glass, stone or coconut shell) in such a way as to control the shape of the scar on various parts of the body [1]. The origins of therapeutic scarification are lost in antiquity and the methods probably developed independently in various parts of the world. A theory was that primitive men probably scratched and sucked diseased and painful parts [2]. The practice of inflicting cuts on the anterior abdominal wall to treat splenomegaly of various causes is a very common one in some parts of west Africa. An example of such places is in Edo State, Nigeria [3]. Other medical indications include: the treatment of epilepsy, febrile convulsions, prevent death as a child, protection from evil spirits and the fear of the unknown. Several non-communicable and infectious conditions may result from scarification. Complications like cutaneous sarcoidosis, filarial elephantiasis, sepsis, HIV, viral Hepatitis and tetanus have been highlighted [4]. In Senegal, 3.6% of all tetanus cases between 1982-1990 occurred in pierced, circumcised, tattooed and scarified individuals [2]. These practices expose these children to physical pain and leads to delay in proper and correct management and puts these children at risk of complications due to the ongoing disease and complications caused by the act of scarification. It is therefore of vital importance that we create awareness in our society that this practice conflicts with timely medical attention. This would also reveal the impact this practice has had on the community, create awareness of its complications and implement simple strategies to stop it. So, we decided to assess the burden, predisposing factors and outcome of scarification among children less than 15 years old in three hospital settings of the Limbe Health District.
Material and Methods
A three-month hospital-based cross-sectional study was carried out from February to April 2022. The areas of study were three hospital settings in the Limbe Health District which were sampled using the convenient sampling method. They were; Limbe Regional Hospital (located at Mile 1 Limbe), Bota District Hospital and Down Beach Health Centre. We included all children ≤15 years old whose parents gave their consent and excluded all neonates (infants <28 days old). The reason being that they were too small and fragile for the act, so the community does not adhere to this practice at this age. An estimated sample size of 269 participants was calculated using COCHRAN statistical formula and participants were recruited using consecutive sample technique. Carers were explained the procedure to get their consent. They were later interviewed directly in the wards pediatric ward and Outpatient Department (OPD). The patients were equally undressed and a thorough dermatologic exam was carried out to identify suspicious scars. A structured questionnaire was used to collect data from each parental participant. Data was entered using epidata software and exported to the Statistical Packages for Social Sciences (SPSS) version 26. Categorical variables (qualitative data): sex, address, income, religion etc., were summarized using frequencies and percentages. A binomial logistic regression statistical test was used for group comparisons of categorical variables and a multinomial logistic regression was used to exclude confounders. A p-value <0.05 was considered statistically significant.
Results
A total of 280 children less than 15 years were approached, but 40neonates were excluded, so 240 participants were included. The ages of the participants ranged from 0.25 years (3 months) to 15.00 years of age with a mean of 4.43 years. The most represented age group was children <5 years old, 151(62.9%) and most were scarified at ages less than 5 years. The males were more represented with 143 (59.6%) against 97 (40.4%) for females (as illustrated in Table 1). Meanwhile, maternal ages ranged from 17 years to 60 years with a mean of 32.81 years. Majority 114(47.5%), of them were between 25 to 35 years old, 114(47.5%) had an income >100000FCFA, 215(89.6%) were Christians, the highest level of education for most was secondary school 104(43.4%) and most lived in urban areas 187 (77.9%). 69.2% of them believed that their child’s illness couldn’t be treated in the hospital.
|
Variables |
Number of Participants, N=240 |
Percentage (%) |
|
Age range(years) <5 5-10 11-15 |
151 70 19 |
62.9 29.2 7.9 |
|
Sex Male Female |
143 97 |
59.6 40.4 |
|
Age of the patient at scarification(years) <5 5-10 >10 Nil |
111 23 3 103 |
46.3 9.6 1.3 42.9 |
Table 1: Socio-demographic characteristics of the children.
Amongst the hospitalized children the most worrisome symptoms to their guardians were fever 231 (96.3%), generalized body weakness 181(75.4%) and tachycardia 99(41.3%) all prompting the act of scarification (Table 2).
|
Variable |
Number of Participants, N=240 |
Percentage (%) |
|
Fever |
231 |
96.25 |
|
Generalized body weakness |
181 |
75.4 |
|
Palpitationsa |
99 |
41.3 |
|
Left-sided abdominal painb |
91 |
37.9 |
|
Clinical anemia |
83 |
34.6 |
|
Nausea/vomiting/diarrhea |
43 |
17.9 |
|
Blood transfusion |
27 |
11.3 |
|
Splenomegaly |
17 |
7.1 |
|
Seizures |
16 |
6.7 |
|
Hepatomegaly |
13 |
5.4 |
|
Right-sided abdominal paina |
9 |
3.7 |
|
Hepatosplenomegaly |
6 |
2.5 |
|
(a) Called “under bobi” by participants; (b) Called “side pain or corner bele” in local terms. Could be left or right. |
||
Table 2: Clinical characteristics of the participants.
The proportion of children with scarification was 137 (57.1%). Ninety-five (69.3%) were located below the left nipple, 104 (75.9%) were mechanical scars (marks from a blade) and 135 (98.5%) were performed by a herbalist under non-sterile conditions (Fig. 1-3).
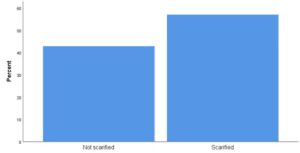
Figure 1: Graphical presentation of the frequency of scarification in the Limbe health district.

Figure 2: A scar highlighted by the yellow circle predominantly chemical inflicted with some degree of thermal element added to it in a 9-month-old infant at the left lower quadrant. (Picture taken in Bota district hospital on 26/03/2022).

Figure 3: 1 year old female with chemical burn (made from herbs grounded to paste) highlighted by the yellow circle at the left lower quadrant of the abdomen. (Picture taken in Bota district hospital on 26/03/2022).
In multivariate analysis, we adjusted for determinants of scarification that had a p-value ≤ 0.05 and having left abdominal pain, palpitations and a scarified sibling were factors predisposing a child to scarifications (Table 3).
|
Variable |
Adjusted Odd Ratio |
95%CI |
P-value |
|
LAP Palpitations GBW Scarified sibling Secondary education Low income level |
7.348 5.504 0.060 5.976 0.231 0.408 |
2.955-18.269 2.357-12.852 0.019-0.192 2.054-17.386 0.089-0.599 0.180-0.922 |
0.00 0.00 0.00 0.001 0.003 0,031 |
|
(a) LAP (Left abdominal pain) ; (b) GBW (General Body Weakness) |
|||
Table 3: Factors independently associated with scarifications.
During our study we had 1(0.7%) HIV infection related to the practice, 3(2.2%) infected sites of scarification and 2(1.5%) death cases due to delay in medical treatment. One died of severe pneumonia complicated by severe respiratory distress and the other had severe sepsis on arrival as per the doctor on call reports.
Discussion
The ages of the participants ranged between 0.25 years (3 months) to 15.00 years of age with a mean of 4.43 years. The most represented age group was children <5 years old, 151(62.9%) and most were scarified at ages less than 5 years. The males were more represented with 143 (59.6%) against 97 (40.4%) for females. The reason for this is that malaria in children <5years old is usually severe than any other age group thus putting children <5years at a greater risk. This study differs slightly from Salami, et al., [5].
Most children had fever 231 (96.25%), generalized body weakness 181 (75.4%), 99 (41.3%) had palpitations, while 91(37.9%) had Left Abdominal Pain. Our results were similar to those of Salami, et al., in Nigeria who had similar symptoms: 75% with fever, followed by 60% with abdominal swelling. With hepatomegaly and or splenomegaly in a febrile context in our community, some parents believe the fever and body weakness is caused by the enlarged liver or spleen, locally called “corner bele” so decide to scarify around that abdominal region to treat the enlarge liver or spleen. On the contrary, Tsiba, et al., had majority of their participants scarified for having a swollen abdomen (40.4%), stunting (20.2%) and (19.3%) for recurrent bronchitis [6].
With respect to the sites and characteristics of the scar, 95 (69.3%) of the participants were scarified below the left nipple and 104 (75.9%) had mechanical scars (scratch marks from a blade). This was because palpitations in a febrile context are generally thought to suffer a condition known to them as “under bobi” which is believed to be treated by making scratch marks on the left hemithorax just below the nipple. This was followed by the left flank (38.7%) and the right flank (24.1%) for the symptomatic treatment of splenomegaly or hepatosplenomegaly respectively and for the symptomatic treatment of abdominal pain. This finding differs from the report of Tsiba, et al., with 82.4% done at the hypochondriac, 14.6% at the flanks and 13.8% at the hemithorax (slightly below the nipple) with the only similarity being the use of a blade in most cases (52.3%) [6].
The prevalence of scarification in our study was 57.1% with a prevalence of 32.1%, 17.5% and 7.5% in Bota District hospital, Mile 1 Regional hospital Down beach health center respectively which is significantly lower to 77.4% from the study conducted by Wagbatsoma, et al., in Nigeria [7]. The main reason for this difference is because their study was a community-based study more so in a rural setting.
Among the predisposing factors, scarification was positively associated with left-sided abdominal pain, palpitations and having a scarified sibling. There was a general believe that having childhood fever associated with palpitation commonly called “under bobi” and abdominal pain still in a febrile context commonly called “corner bele” are diseases that could only be treated by herbalists through scarification. This result shared similarities with that conducted by Salami, et al., but contrary to Tsiba, et al., with majority being scarified for having a swollen abdomen (40.4%), stunting (20.2%) and (19.3%) for recurrent bronchitis [5]. On the other hand, having generalized body weakness, a parent with a higher level of education and a parent with low-income levels, were all negatively associated to scarifications, because the fear of losing the child is higher with general body weakness, so parents will hesitate to carry out the act and the more educated you are, the more knowledgeable you are.
Of all the scarified participants of our study, 1(0.7%) had HIV infection related to the act, 3 (2.2%) had infected fresh wounds at the scar sites and 2(1.5%) death cases: one in LRH (severe pneumonia complicated by severe respiratory distress) and another in BDH (severe sepsis with multiple organ failure). This result is differing largely from that of Salami, et al., with 40% having infections related to scarification with no precision on which type of infection, 10% with keloids and no death case. The main reason for the difference is that their study was community-based study.
Conclusion
The hospital burden of scarification amongst children is relatively high and predisposing factors are mostly linked to the clinical state of the child and having at least 1 scarified sibling. Though very few children were confirmed to suffer from complications, the death of a child due to delay of appropriate treatment is a wakeup call to the weight of community Paediatrics we have to invest in, to save the Paediatric population.
Conflict of Interest
The authors have no conflict of interest to declare.
Financial Disclosers
The authors have no financial relationships relevant to this article to disclose.
Author Contributions
NM conceived the study and drafted the initial manuscript. MK, JT, KD, KK and ME participated in data extraction and analysis. VV and HE reviewed and corrected.
Data Availability Statement
Data available upon written request to the corresponding author.
Acknowledgment
The authors would like to thank the research assistants for data extraction and statistical analysis.
References
Research Article
Received Date: 28-03-2024
Accepted Date: 14-04-2024
Published Date: 22-04-2024
Copyright© 2024 by Monono N, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Monono N, et al. Scarrifications Hospital Review of a Traditional Method of Managing Paediatric Hepatomegaly and Splenomegaly in Three Hospitals in the Limbe Health District, Cameroon. J Pediatric Adv Res. 2024;3(1):1-6.

Figure 1: Graphical presentation of the frequency of scarification in the Limbe health district.

Figure 2: A scar highlighted by the yellow circle predominantly chemical inflicted with some degree of thermal element added to it in a 9-month-old infant at the left lower quadrant. (Picture taken in Bota district hospital on 26/03/2022).

Figure 3: 1 year old female with chemical burn (made from herbs grounded to paste) highlighted by the yellow circle at the left lower quadrant of the abdomen. (Picture taken in Bota district hospital on 26/03/2022).
Variables | Number of Participants, N=240 | Percentage (%) |
Age range(years) <5 5-10 11-15 |
151 70 19 |
62.9 29.2 7.9 |
Sex Male Female |
143 97 |
59.6 40.4 |
Age of the patient at scarification(years) <5 5-10 >10 Nil |
111 23 3 103 |
46.3 9.6 1.3 42.9 |
Table 1: Socio-demographic characteristics of the children.
Variable | Number of Participants, N=240 | Percentage (%) |
Fever | 231 | 96.25 |
Generalized body weakness | 181 | 75.4 |
Palpitationsa | 99 | 41.3 |
Left-sided abdominal painb | 91 | 37.9 |
Clinical anemia | 83 | 34.6 |
Nausea/vomiting/diarrhea | 43 | 17.9 |
Blood transfusion | 27 | 11.3 |
Splenomegaly | 17 | 7.1 |
Seizures | 16 | 6.7 |
Hepatomegaly | 13 | 5.4 |
Right-sided abdominal paina | 9 | 3.7 |
Hepatosplenomegaly | 6 | 2.5 |
(a) Called “under bobi” by participants; (b) Called “side pain or corner bele” in local terms. Could be left or right. | ||
Table 2: Clinical characteristics of the participants.
Variable | Adjusted Odd Ratio | 95%CI | P-value |
LAP Palpitations GBW Scarified sibling Secondary education Low income level | 7.348 5.504 0.060 5.976
0.231 0.408 | 2.955-18.269 2.357-12.852 0.019-0.192 2.054-17.386
0.089-0.599 0.180-0.922 | 0.00 0.00 0.00 0.001
0.003 0,031 |
(a) LAP (Left abdominal pain) ; (b) GBW (General Body Weakness) | |||
Table 3: Factors independently associated with scarifications.