Katie Scott1, Vincent S Gallicchio1*
1Department of Biological Sciences, College of Science, Clemson University, Clemson, SC 29627, USA
*Correspondence author: Vincent S Gallicchio, Department of Biological Sciences, College of Science, Clemson University, Clemson, SC 29627, USA; Email: [email protected]
Published Date: 13-08-2024
Copyright© 2024 by Scott K, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Stem cell therapy used to treat Acute Lymphoblastic Leukemia in adults (ALL) has been one of the more promising uses of stem cells and has large implications on the survival rate of adults with ALL. While the survival rate of ALL remains relatively low at an estimated 20% to 30% in adults, stem cell as an adjunct therapy has shown promising results. Historically, ALL has a high rate of recurrence in adults and one study aims to assess the effectiveness of hematopoietic stem cell therapy in diminishing the rates of recurrence. Stem cell therapy for blood diseases is most found in the form of an allogeneic bone marrow transplant, which includes transplantation of HSCs from a donor. It can help to stimulate the body to produce healthy blood cells and thereby keep the disease at bay. The study concluded that HSCT increases the survival rate of adults with ALL and that it should be considered if a patient has a viable donor available. We see that multiple other studies come to similar conclusions, such as one study that found increased long-term disease-free survival can be achieved through stem cell therapy. A culmination of incredible research excites the idea of an extraordinary step forward in helping to cure those suffering from acute lymphoblastic leukemia and improve long-term, disease-free survival.
Keywords: Acute Lymphoblastic Leukemia; Human Leukocyte Antigen; Hematopoietic Stem Cell Therapy
Abbreviations
ALL: Acute Lymphoblastic Leukemia; AutoSCT: Autologous Stem Cell Transplant; BMT: Bone Marrow Transplantation; CTCT: CAR-T Cell Therapy; GVHD: Graft-Versus-Host Disease; HLA: Human Leukocyte Antigen; HSCT: Hematopoietic Stem Cell Therapy; Ph+: Philadelphia Positive; TKIs: Tyrosine Kinase Inhibitors
Introduction
For years, biomedical research has continually discovered the ever-growing use of stem cells to treat a wide variety of medical conditions, acute lymphoblastic leukemia being one of these conditions. ALL is most diagnosed in children, with it being the leading type of childhood cancer. Children with ALL see a 90% survival rate, which is a stark contrast to the 20% to 30% that adults unfortunately see with this same type of cancer. Symptoms of ALL can vary significantly, but the most frequently observed include fever, bleeding and bruising, pale skin and frequent infection. Although it is the most common childhood cancer, the overall incidence of ALL in adults is uncommon, with approximately 6,000 new cases diagnosed in the current year [1]. When comparing its incidence to other cancers, the relative rate of occurrence is low. Ironically, the rate of recurrence is relatively high in adults with ALL. Therefore, stem cells are being studied to use as a post-remission treatment to decrease likelihood of recurrence [2]. In theory, by replacing the nonfunctional hematopoietic stem cells that are producing immature blood cells with healthy stem cells to produce healthy blood cells, the occurrence of these immature cells can essentially be eradicated. Furthermore, the stem cells also carry antileukemic properties that can help to kill the cancerous cells that are left after induction of remission. Although ALL cases may reflect only a small percentage of all cancer diagnoses, it is an aggressive cancer with higher recurrence rates that prove to be a challenge to cure. In this regard, cutting edge research aimed at finding potential treatment options could be revolutionary for long-term and disease-free survival of all cancer patients.
To understand the implications and use of stem cells to treat diseases such as acute lymphoblastic leukemia, it is important to first understand these incredible cells. Stem cells are undifferentiated cells that can be found in humans at any stage of life, from embryos to adults. They can specialize into any cell and therefore are extremely useful and important when it comes to replacing mutated cells and allowing our bodies to grow. In embryos, they can be found in the inner cell mass of the blastocyst. These stem cells only last here for about three days before they begin to differentiate into one of the three germ layers. These three germ layers include the endoderm, mesoderm and ectoderm and they will eventually form everything in the body. These stem cells are known as embryonic stem cells and are some of the most useful, but ethically questionable stem cells we can extract. Obviously, since they are only found in the embryo, many argue over whether the extraction and use of them is ethical. Due to the nature of these stem cells, by extracting them we are making the embryo non-viable. This poses a large hurdle in scientists’ abilities to find embryonic stem cells to use and research. Fortunately, adult stem cells are much easier and ethically sound to collect. Adult stem cells can be found in the brain, gut, muscle, skin, teeth, bone marrow, blood, adipose tissue and the umbilical cord of any human. They are much more limited in their differentiation capabilities as compared to embryonic stem cells, unfortunately. There are four main types of stem cells: pluripotent, multipotent, unipotent and totipotent [3]. Pluripotent stem cells can differentiate into cells of all germ layers, excluding those of extraembryonic tissue. For further clarification, extraembryonic tissue includes things like the placenta and umbilical cord. Multipotent stem cells can specialize into some, but not all, cells in the body. This is the category that hematopoietic stem cells fall under, which is the main type being used in treatment of ALL. Unipotent stem cells can form only one cell type and finally totipotent stem cells can form all cell types including extraembryonic tissue. Hematopoietic stem cells can differentiate into all blood cell types through a process of differentiation known as hematopoiesis. These can be especially important in helping to treat and cure leukemia because it is a cancer of the blood (Fig. 1).
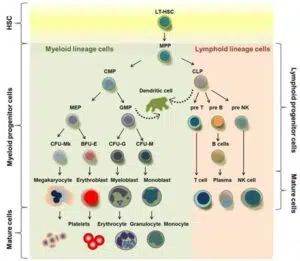
Figure 1: Hematopoietic stem cells and their lineages. Hematopoietic stem cells can give rise to all types of blood cells through a process of differentiation, known as hematopoiesis [4].
Hematopoiesis is the process by which blood stem cells differentiate into the specific types of blood cells [5]. One hematopoietic stem cell could differentiate into a red blood cell, a platelet or any one of the white blood cells. This process occurs in the bone marrow. Hematopoietic stem cells go through multiple steps of differentiation until they eventually reach a mature blood cell and then they are released into the bloodstream. They can be differentiated into myeloid or lymphoid lineage cells. Myeloid cells will then differentiate into erythrocytes, monocytes, granulocytes and platelets. Lymphoid cells will develop into T and B cells, plasma and natural killer cells.
Garnering further insight on acute lymphoblastic leukemia is an essential piece to the puzzle of understanding how stem cells can be used to treat it. ALL occurs when bone marrow starts to release immature lymphocytes, also known as lymphoblasts, into the bloodstream at high rates which can overcrowd healthy blood cells. To properly diagnose this cancer, biopsies and blood tests must be performed. The first line of testing that usually comes after presentation of symptoms are blood tests. A complete blood count can be done to quantify the quantity of lymphocytes in the blood. If physicians observe many lymphoblasts then further testing is ordered. A biopsy of the bone marrow or lymph tissue will then be taken to observe the number of lymphoblasts in the tissues. If the tissue contains more than 20% lymphoblasts, a diagnosis of ALL is typically made [6]. This is a significant increase from the normal 5% blasts that are typically observed. Most of these immature lymphocytes are precursors to B-cells, with the remainder being precursors to T cells [7]. Another hallmark of ALL is the rate at which the disease develops in the body. The term acute is included in its name because it is a rapid onset disease. There are three main types of acute lymphoblastic leukemia: B cell ALL, T cell ALL and Philadelphia-positive ALL [8]. Knowing your type may be crucial in developing a treatment specific to your needs, however the hope is that stem cells can be effective in beating all three types. B cell ALL is the most common type, accounting for about 75% of cases diagnosed. It is the overgrowth of B cell precursors or lymphoblasts. These B cell lymphoblasts are supposed to help you fight off infection, however they can overgrow and spread to other parts of your body. Researchers believe that ALL is not passed down genetically and quite unsure about what causes people to develop it [9]. T cell ALL is distinct from B cell ALL in the fact there is an overgrowth of a different type of lymphoblast, the T cell lymphoblast. It accounts for about 15% of ALL cases and most commonly occurs among pediatric patients. Patients with this type of ALL typically see fewer favorable outcomes as compared to those with B cell ALL [10]. Recent advancements have been made in the treatment process for this type, however, there is still a long way to go and improvements are constantly being researched. Philadelphia-positive (Ph+) ALL occurs in about 30% of adult patients with ALL and poses a greater risk than its Philadelphia negative counterpart. It occurs due to a genetic abnormality, specifically a fusion oncogene, BCR- ABL. This gene encodes an oncogenic protein that constitutively turns on tyrosine kinase [11]. This over activates bone marrow and causes too many lymphoblasts to be produced in a short amount of time. Patients with ALL can have either the B or T cell type and be either Ph positive or Ph negative. Allogeneic stem cell therapy has proven to be effective in treating Ph+ ALL after first remission and therefore leads to more research as to how stem cells can be used to treat all three of the main types.
In treating ALL specifically, hematopoietic stem cells are often used because they can promote the development of normal lymphocytes. Chemotherapy is the first line treatment for ALL, to eradicate the underdeveloped cells. This phase is referred to as the induction phase. During this phase, physicians aim to destroy all the patient’s abnormal cells. This is used to help alleviate patients of symptoms [9]. Then, the post remission phase begins, which is when stem cells are most used. Here, physicians are attempting to kill off any remaining abnormal cells that aren’t actively causing the patient symptoms to assure that they never become active. They also are aiming to restore healthy lymphocytes in the patient’s bloodstream. This stage is critical to help prevent ALL from ever returning. Because we know that this disease in adults has a high recurrence rate, this stage of treatment needs the most improvement. Stem cells can serve to fill that treatment gap. Finally, physicians initiate the maintenance phase for patients in which they are treated with chemotherapy much less intensely as a preventative measure against the cancer. Stem cells prove to be an extremely enticing form for treatment in all types of ALL and researchers are beginning to explore the amazing possibilities it could present more rigorously.
Discussion
In adults with ALL, one of the biggest risks is the rate of recurrence that patients often see. This means post remission treatment options are extremely valuable. There are many treatment options being explored including chemotherapy, CAR-T cell therapy and stem cell therapy. In most cases, the stem cells used to treat ALL come in the form of hematopoietic stem cells and are typically introduced through bone marrow transplantation. Allogeneic stem cell transplants seem to be more beneficial and therefore are selected for many high risk ALL patients. Though not fully researched, stem cells are unquestionably useful in the treatment of ALL. They can be useful with or without combinations of other treatments.
Chemotherapy
Chemotherapy used during post remission proves to be an effective, though intensive, treatment option for those with ALL. Chemotherapy is the mainstream treatment among all types of cancer. It is extremely aggressive on the body and in some cases, it can ultimately lead to death. One study seeked to compare allogeneic Hematopoietic Stem Cell Therapy (HSCT) and chemotherapy effectiveness used during post remission therapy. 158 patients were included in this trial, all having Philadelphia positive ALL. 74 patients were treated with chemotherapy plus tyrosine kinase inhibitors for 2 years. Tyrosine Kinase Inhibitors (TKI’s) work directly against the mutated BCR-ABL1 gene in Ph+ ALL. TKI’s in conjunction with the chemotherapy, produced a 4-year overall survival rate siting at around 63% [13]. The study concluded that the overall survival of those patients who received chemotherapy versus allogeneic stem cell therapy was comparable and the difference was not statistically significant [12]. Though this study yielded comparable efficacy rates of the two treatment types, allogeneic HSCT still remains the mainly selected treatment option during post remission treatment. In most studies, chemotherapy is used as the first treatment to induce post remission in patients. Subsequently, stem cell therapy is then used to help ensure the patients stay in remission.
CAR-T Cell Therapy
Another form of treatment that can accompany stem cell therapy is CAR-T Cell Therapy (CTCT). This version of immunotherapy works to engineer T cells to attack and kill cancer cells in the body. CTCT involves the genetic modification of T cells to allow them to recognize and attack cancer cells [13]. T cells are collected in the lab and are combined with a chimeric antigen receptor so they can locate and identify the cancerous cells. The process of CAR-T cell development can be seen in Fig. 2. This treatment has been used to put patients in remission and allow for an allogeneic bone marrow transplant to then lead them to long-term, disease-free survival [14]. In younger adults, CAR-T cell therapy immediately followed by transplant proves to be an extremely effective treatment option.
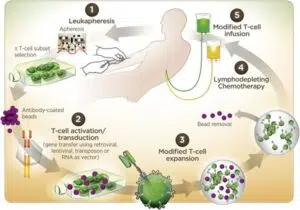
Figure 2: Steps of creating CAR-T cells for use in treatment of ALL [14].
Autologous Stem Cell Therapy
An autologous stem cell transplant (autoSCT) can be an option for some patients diagnosed with ALL. An autoSCT involves the extraction of healthy stem cells from a patient’s blood or bone marrow for use after treatment of the disease, which in this case is ALL. This sort of SCT offers protection from rejection due to the autologous nature of the transplanted cells. Before one undergoes extraction and transplantation, a physician must first assess whether the patient would be a good candidate. There is a comprehensive list of factors that go into this assessment that include things from disease risk factors to prior treatments. Patients most often receive this treatment after recurrence has occurred and it is most often used for cancers deriving from hematopoietic stem cells, one being ALL. Also, physicians will need to determine the patient is equipped to receive such a robust treatment and will be able to withstand potential side effects. In some cases, a patient may have to take medication prior to harvest to increase their stem cell count to provide enough for later transplantation. After all these criteria are reviewed, an autoSCT may be chosen as an effective course of treatment for ALL.
Allogeneic Hematopoietic Stem Cell Therapy
Conversely, an allogeneic stem cell transplant is another and typically preferred, option for treatment of ALL. Allogeneic HSCT is the transplantation of hematopoietic stem cells from another human donor. Allogeneic stem cell therapy is the preferred method of stem cell therapy due to effective antileukemic properties, as shown by a meta-analysis performed to assess the role of HSCT in high risk ALL treatment. It involves matching between donor and recipient based on their Human Leukocyte Antigen (HLA). In most cases, transplantation occurs between individuals who are HLA identical. There are a couple different types of donors, two of the most common being matched sibling donors and matched unrelated donors. In both cases, the HLA for donor and recipient are matched; their relatedness is simply the difference. Before allogeneic stem cell therapy, intensive chemotherapy and eradication must occur to ensure the recipient is in the post remission phase. The specific types of stem cells are then implanted and engraftment occurs. As a result of transplantation, donor cells attack leukemic cells in the recipient’s body helping to eradicate the cancer. This is known as the graft-versus-leukemia effect. Like autoSCT, alloSCT also has selection criteria that is assessed by physicians before this option of treatment is recommended. In most cases, this form of stem cell therapy will be chosen for those in post remission from ALL.
Clinical Evidence
Hematopoietic Stem Cell Therapy (HSCT) poses potentially beneficial implications in long-term treatment for ALL. One study sought to assess their efficacy as a part of post remission treatment for patients with high risk ALL [15]. Researchers found a strong positive correlation between survival and allogeneic HSCT in patients with high risk ALL. However, this study specifically focused on cases of high risk ALL, as defined in Table 1, therefore the efficacy of HSCT in standard risk ALL treatment was not assessed. Additionally, a negative correlation between the duration of complete remission or induction and survival was found. Therefore, HSCT should be considered and implemented as soon as possible in cases where it would be beneficial to increase overall survival [15].
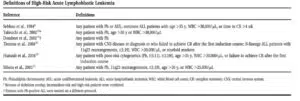
Table 1: Definitions of high risk ALL as defined by multiple studies [15].
As previously mentioned, Bone Marrow Transplantation (BMT) is a form of hematopoietic stem cell therapy since bone marrow is where HSCs reside. Further, it has also already been discussed the front-line status of bone marrow transplantation as a means of treatment for ALL [16]. It serves to replace diseased marrow cells in the patient which can help regenerate new, mature blood and immune cells. One specific study reports the results of bone marrow transplantation in 52 adult patients with ALL [16]. As detailed in Fig. 3, patients who received a BMT during second remission experience a higher overall survival and disease-free survival as compared to those in third remission or relapse. Another study indicates allogeneic BMT as an effective post-remission treatment option for those in remission 1 or 2 [17]. It is also important to consider implications of risk factors such a Ph+, B cell phenotype and high leukocyte counts. Some studies find that BMT can help to mitigate these risk factors and achieve desired outcomes of overall survival [18]. BMT proves to be an effective option to improve recurrence rates and therefore overall survival rates, in patients with ALL.
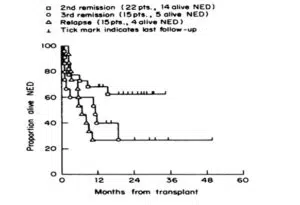
Figure 3: Graph displaying proportion of patients in disease free survival for three study groups: second remission, third remission and relapse [16].
While autologous stem cell therapy can be an effective treatment option in some cases, allogeneic proves to be more commonly effective in specifically treating ALL. In Table 2, the percentage of overall survival is significantly higher, 44% compared to 10%, for allogeneic stem cell therapy. It is worth mentioning, however, this significant difference is only seen in high-risk cases. Standard risk cases see the exact same overall survival rate between allogeneic and autologous therapies.
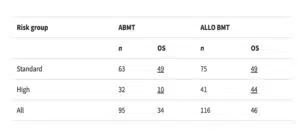
Table 2: Comparison of overall survival percentages between allogeneic and autologous stem cell transplantation in standard and high risk ALL. Underlined numbers are overall survival percentages over 10 years [19].
By pairing both chemotherapy and allogeneic stem cell therapy, a more effective treatment plan could be developed. A study found that eradication with chemotherapy followed by a stem cell transplant during post remission can produce desirable effects of long-term, disease-free survival [20]. Other studies find that the use of both chemotherapy and stem cell therapy during the post remission process can also enhance the effectiveness of both in keeping the patient in remission.
CTCT has also been studied as a therapy that can be used with stem cell transplantation to treat ALL. It was found that the relapse percentage in patients who only used CTCT was 85.7% compared to those who received both CTCT and SCT, where it was 9.5% [14]. Combination therapies may be extremely effective in helping patients to stay in remission. Overall, as many clinical studies have supported, allogeneic stem cell therapy has proven to be an effective way to treat ALL in post-remission by lowering recurrence rates.
Challenges of Stem Cell Therapy in ALL
Hematopoietic stem cell therapy, in the form of bone marrow transplantation, proves to be a promising treatment option for those with ALL. It helps to increase survival rates by replacing diseased marrow cells and fighting off diseased blood cells in recipients. Unfortunately, this treatment also comes with a share of undesired side effects. As with any procedure, there is always an infection risk associated with a stem cell transplant. Not only does the actual procedure pose an infection risk, for months after the transplant, recipients have an extremely weakened immune system which makes them easily susceptible to any form of infection. It is important for those who receive transplants to take protective measures following their transplant to ensure this risk does not become fatal. Additionally, though matching helps to decrease rejection, Graft-Versus-Host Disease (GVHD) provides yet another potentially dangerous implication of BMT. GVHD occurs when the recipient’s T-lymphocytes recognize the donor tissue as foreign and attack it [21]. Our body does not naturally attack lymphocytes due to the presence of our Human Leukocyte Antigens (HLA) on human blood cells. These antigens mark everyone’s blood cells as their own so the immune system doesn’t recognize them as foreign and attack them. In the case of GVHD, though matching HLAs is a part of the transplant process, no match is ever perfect and therefore this disease can occur in some cases. It can cause inflammation throughout many organs in the body. Unfortunately, it can also lead to mortality in those who receive BMT. It is the leading cause of non-relapse related mortality in patients who have received BMT [22]. Graft failure can also occur in some cases, where the transplanted cells simply do not produce new, healthy cells. This can also be a co-morbidity of GVHD. Mortality related to treatment type is much higher in allogeneic stem cell transplants, but they are much more effective at treating ALL when they are successful.
Conclusion
Stem cell therapy has now become one of the most sought after treatments against ALL. Thus far, the focus has been on stem cell therapy in adult cases of ALL. ALL has such a low overall survival rate in adults as compared to children due to these high incidences of disease recurrence. Though most effectively used in the post-remission stage of treatment, earlier administration of the treatment can help to lower the unusually high recurrence rate this disease carries. Interestingly, many studies contradict when exactly treatment should be initiated. Some conclude as soon after induction of remission is completed, while others argue it is more effective during second remission. This may be due to a lack of data on first remission use in that study; however, many reports also found stem cell treatment more effective for those that had high risk cases of ALL. Many times, in standard risk cases, no improvement on long-term, disease-free survival was seen. Though, this could be because the survival rates in these cases were already much higher than in those high-risk cases. Also, a comparison between specific types of stem cell transplantation was made. Autologous versus allogeneic transplantation comparisons proved evidence that allogeneic stem cell therapy was more effective. This sort of therapy eliminates the need for pre-extraction therapies to help to develop healthy stem cells. It also has been proven to have stronger antileukemic properties. Essentially, allogeneic stem cells are shown to be more effective in killing any lingering cancer cells.
Resource Drawbacks
As with many medical treatment options involving donors, there is a shortage of suitable bone marrow donors. Finding a match proves to not be the only challenge, but simply finding someone willing to donate bone marrow. The process can be painful and carries risk of infection for the donor, which for many turns them off to the idea of donating. Still, once a donor can be located and matched, the process of the actual transplant is painful and expensive. Another challenge that many patients face is the lack of resources to support this kind of treatment. Because the treatment is still undergoing heavy research and development, only a limited portion of major hospital systems have the technology and staff to execute the treatment. An incredible amount of funding is required to develop new medical treatments and unfortunately this effective treatment is not available in many areas. In the United States specifically, medical treatment is often extremely expensive and therefore most of the country cannot not afford stem cell treatment.
Advancements and Future Considerations
As with many medical advancements, as time goes on, we continue to discover new treatment options and ways to improve previous ones. Stem cell therapy for ALL has made large strides over recent years. By refining selections for both donors and patients’ treatment efficacy can be improved. This could help to match donors and recipients more specifically and to help eliminate less suitable donors. Furthermore, other drugs and therapies, such as TKI’s in Ph+ ALL, could be developed to use with stem cell therapy to enhance its results. In some studies chemotherapy is used alongside SCT, which could become a common modality in ALL treatments. Researchers are also working on developing technology to target stem cells that are causing the leukemia, to allow the preservation of normal hematopoietic stem cells. These may be targeted through molecular markers. The goal of researchers is to see improvements in relapse rates. Not only will further discoveries aid in treatment, but improvements in effectiveness of existing stem cell treatments for ALL can bring immense help. One way this can be done is by increasing the graft-versus-leukemia effect of stem cells. By enhancing T-cell functioning or modifying immune checkpoints, the leukemic effect of transplanted cells can be augmented. Finally and potentially most importantly, transplantation related mortality can be improved upon. By improving infection rates and mitigating GVHD, stem cell therapy can be given a chance to have long term beneficial effects for ALL patients. Stem cell research has only discovered a small fraction of what can be done and there will only be improvements in treatment for ALL.
Final Remarks
In simple terms, replacing diseased bone marrow with healthy bone marrow makes for quite a logical treatment option of this ravaging disease. Unfortunately, the implications of stem cell therapy go much deeper than this. Despite all the challenges that accompany stem cell therapy for ALL, it provides hope for further advancement of techniques that will one day be used widespread to help patients achieve disease-free, long-term survival.
Conflict of Interests
The authors have no conflict of interest to declare.
References
Review Article
Received Date: 18-07-2024
Accepted Date: 06-08-2024
Published Date: 13-08-2024
Copyright© 2024 by Scott K, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Scott K, et al. Stem Cell Treatment for Acute Lymphoblastic Leukemia in Adults J Reg Med Biol Res. 2024;5(2):1-9.

Figure 1: Hematopoietic stem cells and their lineages. Hematopoietic stem cells can give rise to all types of blood cells through a process of differentiation, known as hematopoiesis [4].

Figure 2: Steps of creating CAR-T cells for use in treatment of ALL [14].

Figure 3: Graph displaying proportion of patients in disease free survival for three study groups: second remission, third remission and relapse [16].

Table 1: Definitions of high risk ALL as defined by multiple studies [15].

Table 2: Comparison of overall survival percentages between allogeneic and autologous stem cell transplantation in standard and high risk ALL. Underlined numbers are overall survival percentages over 10 years [19].