The Use of Intra-Operative Brilliance Amplifier by Novice Surgeons to Improve Bone Tunnels Placement in Anterior Cruciate Ligament Reconstruction during Residency Curriculum: Useful or Not?
Hatim Abid1*, Mohammed El Idrissi1, Abdelhalim El Ibrahimi1, Abdelmajid Elmrini1
1Department of Osteoarticular Surgery B4, Hassan II Teaching Hospital, Fes, Morocco
*Corresponding Author: Hatim Abid, Department of Osteoarticular Surgery B4, Hassan II Teaching Hospital, Fes, Morocco; Email: hatim.abid1@gmail.com
Citation: Abid H, et al. The Use of Intra-Operative Brilliance Amplifier by Novice Surgeons to Improve Bone Tunnels Placement in Anterior Cruciate Ligament Reconstruction during Residency Curriculum: Useful or Not ? Jour Clin Med Res. 2022;3(3):1-7.
Copyright© 2022 by Abid H, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 12 Aug, 2022 | Accepted 30 Aug, 2022 | Published 06 Sep, 2022 |
Abstract
Objective: Our objective was to evaluate the contribution of the use of intra-operative fluoroscopy on tunnels positioning during the Anterior Cruciate Ligament (ACL) reconstruction.
Methods: Between January 2020 and June 2022, a total of 8 ACL reconstructions by the Kenneth Jones (KJ) technique were performed by the same young orthopedic surgeon. Fluoroscopy was used intraoperatively to control the position of the guidewire before bone tunnels reaming. It was available for use in 4 cases who constituting the Fluoroscopy Assisted Reconstruction Group (FARG). Post operatively, we assessed on plane radiographs the interference screws position of the four patients constituting the Fluoroscopy Free Reconstruction Group (FFRG). The measurements of the two groups were compared and analyzed using a Wilcoxon matched-pairs signed-ranks test.
Results: Of the 4 patients operated on using intra operative fluoroscopy, imaging allowed us to reposition the tibial and femoral guide wires before reaming in all cases (100%). In the second group (FFRG) of patients (n=4), operated without fluoroscopy, post-operative screw positions were in all patients (100%), more anterior in the tibia and more posterior in the femur than the usual position of bone tunnels of ACL reconstruction.
Conclusion: In order to increase the precision of the bone tunnels placement during ACL ligamentoplasty in the hands of novice orthopedic surgeon, intraoperative fluoroscopy constitutes a considerable aid tool.
Keywords
Anterior Cruciate Ligament; Ligamentoplasty; Intra-Operative Fluoroscopy; Novice Orthopedic Surgeon, Residency Curriculum
Introduction
The precision in the placement of the bone tunnels in isometric position is essential for the clinical and functional success of the ACL ligamentoplasty [1-3]. This necessarily involves a long learning curve and is acquired with practice. On this subject, the literature review highlights significant variations in the placement of the bone tunnels without there being any correlation with expertise level of the surgeons [4-6].
In our Moroccan context, where ACL ligamentoplasty is burgeoning with the increased number of sports and public road accidents, the acceleration of learning this procedure with the necessary mastery for optimal bone tunnels positioning can pass, in the absence of veritable simulation exercise in the residency curriculum, through the use of intra-operative fluoroscopy.
Patients and Methods
Between January 2020 and June 2022, eight patients were followed prospectively for ACL injury operated by the same novice orthopedic surgeon by the Kenneth Jones technique. The brilliance amplifier was used in 4 patients. The procedure was performed using a standard patellar tendon graft. In lateral imaging, the brilliance amplifier allows instantaneous control of the paths of the guide wires both at the tibial and femoral level. Thus, the guide wires trajectories are corrected if necessary before reaming. The comparison was made between reamers position in the patients (n=4) controlled intraoperatively with the brilliance amplifier and that of the interference screws in the patients (n=4) operated without recourse to fluoroscopy. Clinically, patients were assessed at different times (6 weeks, 3 and 6 months) by the International Knee Documentation Committee (IKDC) knee evaluation score [7] and Tegner activity score [8]. Our demographic characteristics and imaging measurements were reported as mean and compared using a Wilcoxon matched-pairs signed-ranks test. A p-value < 0.05 was considered statistically significant. This study respected ethical requirements in clinical research. All patients were asked to give informed consent and confidentiality was ensured. The electronic data has been stored in a password-protected computer.
Results
The Fluoroscopy Assisted Reconstruction Group (FARG) comprised 4 patients (3 men and 1 woman) whose average age was 34 years (22 to 50). In the same way, the Fluoroscopy Free Reconstruction Group (FFRG) comprised 4 patients who were all men and whose average age was 33 years (21 to 48).
The mean tourniquet time was 68 minutes (55 to 80) and 62 minutes (50 to 72) for the fluoroscopy assisted reconstruction group and the fluoroscopy free reconstruction group respectively.
At functional level, the four patients of the FARG were satisfied with a mean IKDC score and mean Tegner activity score of 82 and 6.2 respectively. The results for the patients of FFRG were also good. Their IKDC and Tegner scores were 80 and 5.8 respectively (Table 1).
Under brilliance amplifier, the tibial and femoral guide wires positions were unsatisfactory in the 4 patients (100%) of the FARG. Thereby, the wires were re-positioned before bone tunnels reaming. In this cases, the tibial tunnel was a mean of 41% along the tibial plateau (Fig. 1) and the femoral tunnel was a mean of 80% along Blumensaat’s line (Fig. 2).
Concerning the FFRG, the mean position of interference screws on postoperative radiographs was respectively 28% along the tibial plateau and 88% along Blumensaat’s line. The screws were more posterior at the femoral level and more anterior at the tibial level than the usual tunnels position. The difference between the two groups was significant concerning tunnels position (p = 0.032) (Table 2).
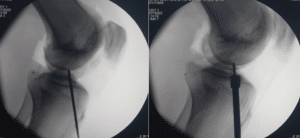
Figure 1: Intra-operative fluoroscopic image showing the guide wire re-positioning followed by the tibial tunnel reaming.
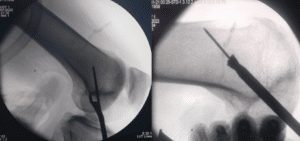
Figure 2: Intra-operative fluoroscopic image showing the guide wire re-positioning followed by the femoral tunnel reaming.
| Fluoroscopy Assisted Reconstruction | Fluoroscopy Free Reconstruction | P-value |
Age Mean (years) | 34 | 33 | 0.85 |
Gender-(Female/Male) | 1/3 | 0/4 | 0.31 |
Body Mass Index kg/m2; Mean | 25.3 | 25.2 | 0.25 |
Follow-up Duration Month; Mean | 10 | 9.3 | 0.63 |
IKDC Score (Postop); Mean | 82 | 80 | 0.42 |
Tegner Activity Score; Mean | 6.2 | 5.8 | 0.13 |
Table 1: Demographic and clinical characteristics of the patients.
Fluoroscopy Assisted Reconstruction Group (n=4) | Fluoroscopy Free Reconstruction Group (n=4) | P-value | ||
Reamer position in the tibia (mean) | Reamer position in the femur (mean) | Screw position in the tibia (mean) | Screw position in the femur (mean) | 0.032 |
41% | 80% | 28% | 88% | |
Table 2: Intra-operative and post-operative measurements of reamer and screws positions.
Discussion
In the United States of America (USA), the annual incidence of the ACL injury turns around 100000-200000 cases. This implies approximatively 400000 ACL ligamentoplasty in worldwide. Generally, this procedure aims to restore the normal knee anatomy and kinesiology [9,10].
The tibial and femoral tunnel placements are of primordial importance in achieving this outcome. Bone tunnels should be positioned as anatomically as possible to prevent many complications which were descripted in previous studies namely impingement, graft stretching or restriction of motion of the knee [10].
Anatomically, The ACL whose center is located around 9 mm posterior to the intermeniscal ligament, extends from the posteromedial aspect of the lateral femoral condyle to the anterior aspect of the tibial plateau. It is characterized by an average intra-articular length and width of 33 mm and 11 mm respectively. The cross sectional area varies according to gender, it is an average 47 mm in males and 37 mm in females [11-14].
In practice, the failure of the ACL ligamentoplasty and bone tunnel-related complications are often related to the incorrect placement of the latters. Posterior placement of femoral tunnel exposes to the risk of posterior wall blow-out during femoral tunnel drilling. Anterior placement of the tibial tunnel often generates a graft impingement [1,2,15].
In the literature, many authors report the absence of correlation between tunnel positioning and surgical expertise. About that, Behrend, et al., noted in their study including 50 patients, correct placement in only 64% of knees [16]. However, recent studies have particularly studied tunnel placement after the ACL reconstruction in relation to surgeon’s practice of this procedure and demonstrated that high surgical volume and experience promote an anatomic tunnels placement [17].
To address issues with tunnel positioning, several techniques and procedures have been developed. The navigational system and orthopedic surgical robot constitute the top of the technological advances in the matter. They allow to increase the bone tunnels positioning precision in an indisputable way [18].
In developing countries as in our case, the brilliance amplifier can be a real therapeutic alternative. During ACL ligamentoplasty, using the brilliance amplifier intra-operatively influences the course of the surgery. On this point, Mehta, et al., were brought to change in their series, the femoral tunnel entry point in 15% of 407 procedures [19]. In the same context, Hughes, et al., corrected in also 15% of their patients thanks to intra-operative brilliance amplifier the unsatisfactory tibial tunnel position [20].
The present study, which is intended for novice orthopedic surgeons shows the technical and pedagogical interest of intra-operative fluoroscopy in the optimization of femoral and tibial bone tunnels positioning during ACL reconstruction surgery. This finding, although approved by other previous studies, should be considered with caution because of our small number of patients.
Conclusion
Intra-operative fluoroscopy used for optimizing bone tunnels placement in ACL reconstruction is a real and reproducible pedagogic tool that we intend to systematically integrate into the residency training curriculum while waiting to develop our simulation teaching programs.
Conflict of Interest
The authors declare no conflict of interests.
References
- Khalfayan EE, Sharkey PF, Alexander AH, Bruckner JD, Bynum EB. The relationship between tunnel placement and clinical results after anterior cruciate ligament reconstruction. Am J Sports Med. 1996;24:335-41.
- Pinczewski LA, Salmon LJ, Jackson WF. Radiological landmarks for placement of the tunnels in single-bundle reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 2008;90(B):172-9.
- Barrett GR, Treacy SH. The effect of intraoperative isometric measurement on the outcome of anterior cruciate ligament reconstruction: a clinical analysis. Arthro. 1996;12:645-51.
- Topliss C, Webb J. An audit of tunnel position in anterior cruciate ligament reconstruction. Knee. 2001;8:59-63.
- Kohn D, Beusche T, Caris J. Drill hole position in endoscopic anterior cruciate ligament reconstruction: results on an advanced arthroscopy course. Knee Surg Sports Traumatol Arthrosc. 1998;6:13-5.
- Allen CR, Griffin JR, Harner CD. Revision anterior cruciate ligament reconstruction. Orthop Clin North Am. 2003;34:79-98.
- Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The international knee documentation committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34:128-35.
- Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-9.
- Hoogeslag RAG, Brouwer RW, Boer BC, de Vries AJ, Huis In ‘t Veld R. Acute anterior cruciate ligament rupture: repair or reconstruction? two-year results of a randomized controlled clinical trial. Am J Sports Med. 2019;47(3):567-77.
- Rayan F, Nanjayan SK, Quah C, Ramoutar D, Konan S, Haddad FS. Review of evolution of tunnel position in anterior cruciate ligament reconstruction. World J Orthop. 2015;6(2):252-62.
- Petersen W, Tillmann B. Anatomy and function of the anterior cruciate ligament. Orthopade. 2002;31:710-8.
- Ferretti M, Doca D, Ingham SM, Cohen M, Fu FH. Bony and soft tissue landmarks of the ACL tibial insertion site: an anatomical study. Knee Surg Sports Traumatol Arthrosc. 2012;20:62-8.
- Giuliani JR, Kilcoyne KG, Rue JP. Anterior cruciate ligament anatomy: a review of the anteromedial and posterolateral bundles. J Knee Surg. 2009;22:148-54.
- Longo UG, Buchmann S, Franceschetti E, Maffulli N, Denaro V. A systematic review of single-bundle versus double-bundle anterior cruciate ligament reconstruction. Br Med Bull. 2012;103:147-68.
- Wolfson TS, Mannino B, Owens BD, Waterman BR, Alaia MJ. Tunnel management in revision anterior cruciate ligament reconstruction: current concepts. Am J Sports Med. 2021;12:3635465211045705.
- Behrend H, Stutz G, Kessler MA, Rukavina A, Giesinger K, Kuster MS. Tunnel placement in Anterior Cruciate Ligament (ACL) reconstruction: quality control in a teaching hospital. Knee Surg Sports Traumatol Arthrosc. 2006;14:1159-65.
- Hughes JD, Gibbs CM, Almast A, Atte A, Sansone M, Karlsson J, et al. More anatomic tunnel placement for anterior cruciate ligament reconstruction by surgeons with high volume compared to low volume. Knee Surg Sports Traumatol Arthrosc. 2022;30(6):2014-9.
- Ding G, Yang G, Zhang J, Huang H, Du J, Ren S, et al. Feasibility and accuracy of orthopaedic surgical robot system for intraoperative navigation to locate bone tunnel in anterior cruciate ligament reconstruction. Int J Med Robot. 2022;18(2):e2354.
- Mehta VM, Paxton EW, Fithian DC. Does the use of fluoroscopic and isometry during anterior cruciate ligament reconstruction affect surgical decision making? Clin J Sport Med. 2009;19:46-8.
- Hughes AW, Dwyer AJ, Govindaswamy R, Lankester B. The use of intra-operative fluoroscopy for tibial tunnel placement in anterior cruciate ligament reconstruction. Bone and Joint Res. 2012;10(1):234-7.
This work is licensed under Attribution-NonCommercial-NoDerivs 2.0 Generic (CC BY-NC-ND 2.0) International License. With this license readers are free to share, copy and redistribute the material in any medium or format as long as the original source is properly cited.

