Home » Lamelar Ichthyosis
Case Article | Vol. 2, Issue 3 | Journal of Clinical Medical Research | Open Access |
Lamelar Ichthyosis
Adelia Wuri Pramudita1, Prasetyadi Mawardi1*
1Department of Dermatology and Venereology, Faculty of Medicine Sebelas Maret University, Dr. Moewardi General Hospital, Surakarta, Indonesia
*Corresponding Author: Prasetyadi Mawardi, Department of Dermatology and Venereology, Faculty of Medicine Sebelas Maret University, Dr. Moewardi General Hospital, Surakarta, Indonesia;
Email: prasetyadi_m@staff.uns.ac.id
Citation: Mawardi P, et al. Lamelar Ichthyosis. Jour Clin Med Res. 2021;2(3) :1-11.
Copyright© 2021 by Mawardi P, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 17 Sep, 2021 | Accepted 08 Oct, 2021 | Published 15 Oct, 2021 |
Abstract
Background: Lamellar Ichthyosis (LI) is a rare hereditary autosomal recessive disease with a defect in chromosome 14q11 which generates defect of transglutaminase-1 (TGM-1) enzyme. Clinical manifestation of IL is initiated with the occurrence of collodion membrane that sheds and is subsequenly replaced by thick scale, eclabium, ectropion, and palmoplantar hyperkeratosis. Gold standard of LI diagnosis is genetic analysis examination. Ichthyosis therapy includes scales removal, topical keratolytic, oral retinoid, and its complication management.
Case: A boy of 3 years and 11 months old was referred from Paediatric Polyclinic to Dermatology and Venereology Polyclinic of Dr. Moewardi Hospital, Surakarta with an ailment of scales all over his body. The scales have appeared since birth. The patient was born encased by a membrane that subsequently shed in a few days, afterward the skin almost all over his body got dry, thicken, and scally like a fish. His eyelids turned outward, and the lips pulled backward. During dermatology examination it was discovered that lamellar type squama with erythematosus basis was visible upon the generalisata regio, hyperkeratosis with a part of erosion and fissure was visible upon bilateral palmar manus et plantar pedis regio. Ectropion was visible upon bilateral oculi regio, eclabium was visible upon oris regio. The result of histopathology examination indicated stratum corneum orthokeratosis, focal parakeratosis upon hypergranulosis and a spectrum of mild psoriasiform hyperplasia. The patient was diagnosed with ichthyosis lamellar and obtained topical therapy of milk bath as well as other therapies for the complications he suffered from.
Discussion: Lamellar ichthyosis is a genetic autosomal recessive skin disease which appears at birth in the form of collodion membrane that covers all over body. Transglutaminase (TGM) 1 gene is reported to be the most frequent gene that undergo mutation in IL. Transglutaminase serves as the catalyst of cellular protein bond in the formation of cornification sheath and ceramide adhesion on lamellar bodies, that it plays an important role in the formation of lipid component and corneum stratum protein. Damage on TGM-1 generates disturbance in the function of skin barrier as it is observed in IL clinical. The therapies applied for IL included scales removal, topical therapy in the form of keratolytic, oral therapy in the form of retinoid, and other advanced management.
Keywords
Ichthyosis Lamellar; Congenital; ARCI; Scales; TGM-1
Introduction
Ichthyosis is a skin disease in the form of scales all over the body without the occurrence of erythema. Lamellar ichthyosis is a genetic autosomal recessive skin disease that appears at birth in the form of collodion membrane which covers all over body of the baby. Lamellar ichthyosis is one of the three genetic skin disorders called Autosomal Recessive Congenital Ichthyosis (ARCI) [1]. The disorder is generated by gene mutation which is located in chromosome 14q11 that serves to code Transglutaminase 1 (TGM-1) enzyme synthesis [2]. Transglutaminase 1 serves to catalyze cellular protein bond and serves in the formation of lipid component as well as protein in stratum corneum [3].
Global LI prevalence is 1 case per 138.000 up to 300.000 births [4]. Kurosawa, et al., in 2018 in Japan reported 30 LI cases of out a total of 220 ARCI cases discovered between 2005-2009 [5]. A study by Suraiyah, et al., in the Departement of Dermatology and Venereology, the Division of Pediatric Dermatology, Faculty of Medicine Universitas Indonesia/Cipto Mangunkusumo Hospital during 2001 to May 2006 discovered 18 cases of ichthyosis with 10 cases (56%) of ichthyosis vulgaris (IV), 6 cases (33%) of LI and 2 cases (11%) of non-bullous congenital ichthyosiform erythroderma [6].
Lamellar Ichthyosis is characterized by thick and grey or brown squama that covers all over body. Infants with LI usually were born encased with collodion membrane that is a semi-translucent which sheds within 10-14 days and is replaced by thick scales [1,7]. Children with severe LI may get eclabium, ectropion, and palmoplantar hyperkeratosis [4,8]. Hyperkeratosis may disturb the functions of normal sweat glands hence it generates hypohidrosis [3,9]. LI diagnosis is based on the clinical description, detailed patients’ and family’s medical history, histopathology examination and genetic analysis [1]. At the moment, genetic analysis is a gold standard in diagnosing LI. There are 8 genes that are involved in LI, namely: ABCA12, lipoxygenase‐3 (ALOXE3), 12R‐Lipoxygenase (ALOX12B), Ceramide synthase 3 (CERS3), Cytochrome P450, family 4, subfamily F, polypeptide 22 (CYP4F22), NIPA‐like domain containing 4 (NIPAL4/ICHTHYIN), Patatin‐like phospholipase domain‐containing protein 1 (PNPLA1) and Transglutaminase 1 (TGM1). Mutation in TGM1 and ABCA12 are reported as the most frequently generate LI [1].
Differential diagnosis of LI are Ichthyosis Vulgaris (IV) and ichthyosis linked to recessive chromosome X. Ichthyosis vulgaris is a disorder generated by mutation in filaggrin genes that serve toward keratinocyte differentiation. Ichthyosis vulgaris is characterized by xerosis, squama, pruritus and greatly related to atopic condition. Predilection of IV on the extensor side of lower leg and back, with chest and stomach area rarely involved. IV manifestation appears at the age of 2 months and gets better during summer [10,11]. Ichthyosis linked to recessive chromosome x is a genetic disorder generated by mutation of Steroid Sulfatase (STS) enzyme characterized by clinical manifestation heavier than IV, in the form of dark brown squama which spreads all over body. The lost of STS function generates hyperkeratosis retention on epidermis [10,12].
LI management principles is removing the scales and repairing skin barrier. The applicable therapy modality is in the form of topical agent such as moisturizer, vitamin D derivative, and keratolytic, as well as oral agent such as oral retinoid [4]. The first line therapy for LI is the application of moisturizer to maintain and repair skin barrier. Glycerol, urea, and propylene glycol are moisturizer substances that are often used. The substances can be mixed with topical keratolytic to improve therapy effectiveness. Anti-keratinization such as tazarotene and vitamin D derivative (calcipotriol) can be added for more severe cases however they should be carefully applied to prevent systemic absorption. The recommended maximum dosage of topical calcipotriol is 5 mg per week for adult (equal to 100 gram of cream) [11]. The frequently used oral retinoid is isotretinoin (dosage 1 mg/kgBW/day) or acitretin (0,5 mg/kgBW/day) [13]. Complications that may occur in LI are thermoregulatory disorder, secondary bacterial infection, and cicatricial alopecia. The appropriate and regular application of first line medications may reduce the complication occurrence [4]. The case report aims to enhance knowledge and improve ability in LI diagnosis and management.
Case
A boy of 3 years and 11 months old was referred from Paediatric Polyclinic to Dermatology and Venereology Polyclinic of Dr. Moewardi Hospital, Surakarta with an ailment of scales all over his body. Based on alloanamnesis of patient’s parents, the scales have been coming up since birth. Initially, patient was born encased by a membrane which shed slowly, subsequently the skin all over body got dry, thicken, and scaly like a fish. The parents also stated that the patient’s eyelids were turned outward, and the lips were pulled backward. The ailments caused patient unable to fully close his eyes and mouth hence it generated watery eyes and dry mouth. Patient did not experience hearing impaired and there is no defecating and urinating problem.
Previously patient had got treatment in Sukoharjo Regional General Hospital for his skin ailments and obtained ointment and moisturizer however the parents did not know the name of the medicines. There was no improvement during the treatment in Sukoharjo Regional General Hospital. Patients is the first child, born spontaneously at gestational age of 31 weeks in Sukoharjo Regional General Hospital with birth weight 1700 gram and birth length 49 cm. At birth the patient underwent mild asphyxia and was referred to neonates High Care Unit (HCU) of Dr. Moewardi Regional General Hospital. The patient was under intensive treatment for 26 days. In pregnancy history, patient’s mother regularly conducted antenatal care in a midwife practice clinic and underwent ultrasound examination and yet did not find any abnormality. There was no family member who suffered from the similar ailments (Fig. 1).
Physical examination revealed that visually the general condition was mildly sick, the consciousness was compos mentis, the pulse was 110 times per minute, the respiration was 20 times per minute, temperature was 37°C, the weight was 13 kilograms, the height was 98 cm and Body Mass Index (BMI) was 13.5 kg/m2. Based on growth diagram the patient’s height and weight were in within normal limit. Dermatology examination discovered lamellar type squama with erythematosus base was visible upon generalisata region, hyperkeratosis with a part of erosion and fissure upon bilateral palmar manus et plantar pedis region. Ectropion was visible upon bilateral okuli region, eclabium was visible upon oris region and tapered fingers was visible upon bilateral fingers region (Fig. 2).
Differential diagnosis of the patient was lamellar ichthyosis, ichthyosis vulgaris dan recessive ichthyosis linked to chromosome X. Afterward, laboratory investigation and histopathology examination to diagnose were performed toward the patient.
Routine blood test revealed hemoglobin 12,2 g/dl (reference value: 14,0- 17.5 g/dl), hematocrit 35% (reference value: 33-45%), leucocyte 10 thousand/ul (reference value: 4,5-14,5 ribu/ul), thrombocyte 356 thousand/ul (reference value: 150-450 thousand/ul), erythrocytes 4,90 million/ul (reference value: 3,80-5,80 million/µl). For diff count the results were neutrophile 55% (reference value: 29-72%), lymphocyte 25% (reference value: 33-48%), monocyte 0% (reference value: 0-6%), eosinophile 0% (reference value: 0-4%), basophile 0% (reference value: 0-1%), PT and APTT within normal limit therefore it could be concluded that the laboratory result of routine blood test was within normal limit.
In histopathology examination which was taken through biopsy of tissue in extensor lower left arm region by Hematoxylin and Eosin (HE) staining on epidermis layer, it revealed the visual of hyperkeratosis with focal parakeratosis and hypergranulosis with mild psoriasiform hyperplasia as well as dermis layer within normal limit (Fig. 3).
The management applied for the patient was in the form of vaselin album smeared 2 times a day in the morning and in the afternoon, olive oil smeared every 1-2 hours and medication with NaCl 0.9% rub 2 times a day for 15 minutes and smeared with gentamicin ointment afterward onto the areas with erosion and fissures. Patients was suggested to bathe with water and pure cow milk with comparison of 1:10 liter once every 2-3 days. The patient was consulted to ophthalmologist and diagnosed with dextral and sinistral ectropion and was given a therapy with one drop of cendo lyteer 2-3 times a day to prevent keratitis and chloramphenicol ointment cream to be smeared onto eyelids to reduce the stiffness of the eyelids. The patient showed an improvement characterized by the improvement on squama after 4 weeks of treatment and improvement on ectropion and eclabium (Fig. 4).
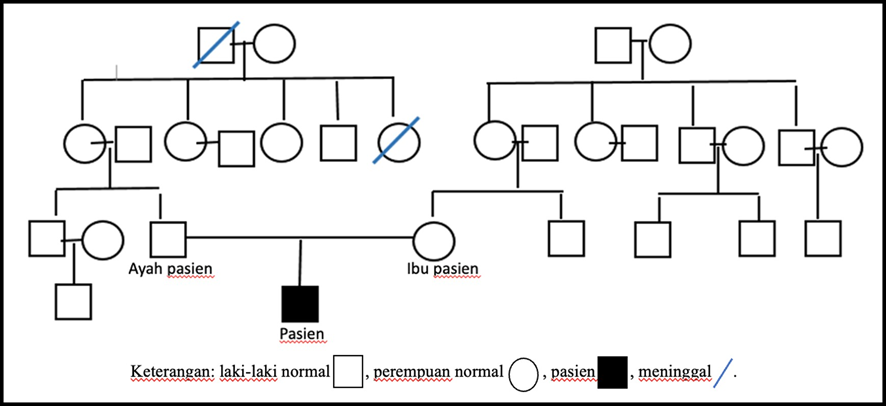
Figure 1: Patient’s family tree in which only patient who suffer from lamellar ichthyosis.
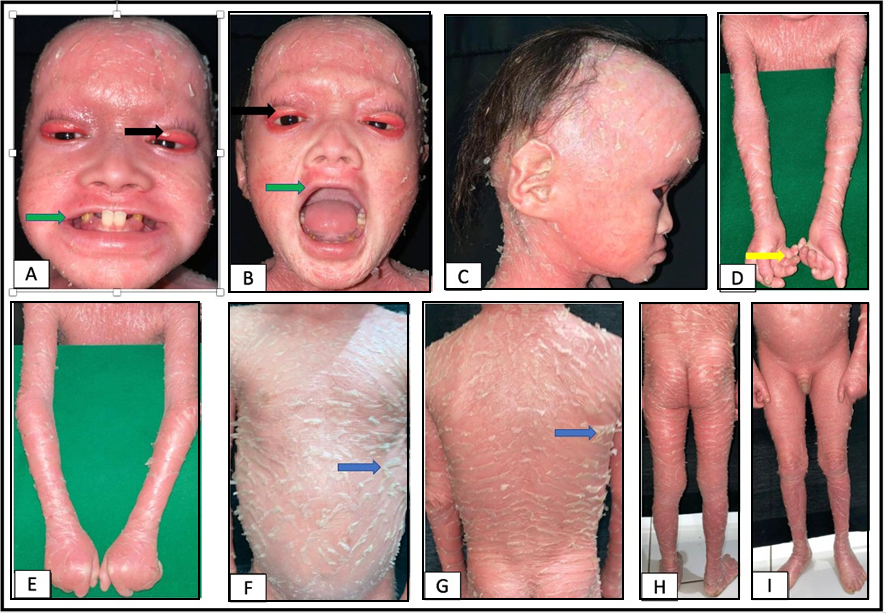
Figure 2: A-C: Bilateral ectropion was visible upon orbital region (black arrow) and eclabium was visible upon oris region (green arrow); D-I: Tapered fingers were visible upon bilateral fingers region s (yellow arrow) and patch erythema were visible upon generalisata region along with thick squama (blue arrow) above.
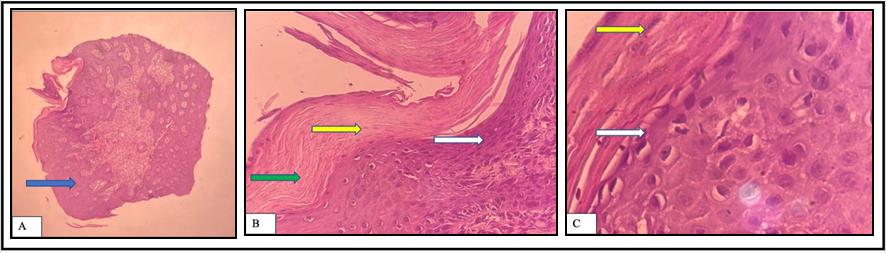
Figure 3: A: The image of patient’s histopathology skin biopsy discovered hyperplasia pseudopsoriasiform (blue arrow) (HE 4x); B: hyperkeratosis (green arrow), focal parakeratosis (yellow arrow), hypogranulosis (white arrow) were visible in epidermis (HE 10x); C: The image of epidermis histopathology discovered focal parakeratosis (yellow arrow) and hypergranulosis (white arrow) (HE 40x).

Figure 4: A-C: Clinical appearance after treatment. Improvement on ectropion (black arrow) upon bilateral orbita region and improvement on eclabium (green arrow) upon oris region; D-I: Improvement on squama (blue arrow) upon generalisata region.
Discussion
Lamellar ichthyosis is a genetic autosomal recessive skin disease that appear at birth in the form of collodion membrane that covers all over body of an infant. Lamellar ichthyosis is generated by gene mutation located in chromosome 14q11 that serves to code Transglutaminase 1 (TGM-1) enzyme synthesis [2]. IL global prevalence is 1 case per 138,000 to 300,000 births. Lamellar Ichthyosis appears since birth and will continue a life time. There is no difference on LI incidence between men and women [4]. In LI the genetic predisposition in the family which indicates chromosome 14q11 abnormality is located in TGM1 gene locus [4].
LI pathogenesis is an epidermis skin barrier defect that generates the decreased function of skin in general [3]. The mutated gene in LI is TGM-1 gene locus that serves in the formation of lipid and protein component in corneum stratum. TGM-1 gene is located in chromosome 14q11. TGM-1 gene serves to catalyze the cellular protein bond, including involucrin, loricrin, small protein that is rich with proline, keratin, and filaggrin during the formation of corneum stratum. The protein complex will deposed into plasm membrane creating cornification sheath. Transglutaminase 1 also functions in ceramide adhesion in lamellar body, therefore the role is essential in the formation of protein and lipid component of corneum stratum [3].
LI clinical description is hyperkeratosis and the occurrence of squama. The characteristics of squama in LI are covers all over body, layered, large, thick, greyish or brown. Ectropion is frequently found on the eyes and eclabium on the mouth. Generally LI is not accompanied by erythroderma. LI patients also often have palmoplantar keratoderma. From alloanamnesis in the case it was discovered that the ailment of thick scales all over body has appeared since birth accompanied by collodion membrane. Dermatology examination revealed that lamellar type squama was visible upon generalisata region with erythematosus base, hyperkeratosis with a part erosion and fissure was visible upon bilateral palmar manus et plantar pedis. Ectropion was visible upon bilateral oculi region and eclabium was visible upon oris region.
Complications that often arise from IL include ectropion of the eye and eclabium of the lips [14]. Such children with IL have bilateral cicatricial ectropion. This occurs due to excessive dryness of the skin and also due to contractures [15]. Ectropion is characterized by eversion of the palpebral conjunctiva and exposing the lids. Cicatrical ectropion is caused by shortening of the anterior lamella of the eyelid, but it can also be caused by certain skin conditions, one of which is lamellar ichthyosis [16]. Ectropion if left unchecked can add to the problem, as it can cause your perforation. This can happen because the ectropion of the environment is in an open condition and is directly exposed to the outside environment. In addition, the presence of defects in storage can add to other problems that can interfere with vision function. Visual function can be decreased or totally blind [17].
Other complications of lamellar ichthyosis include growth failure and rickets vitamin D deficiency [18,19]. Ichthyosis has been reported increase the risk of rickets and vitamin D deficiency several-fold. In addition, growth failure in patients with ichthyosis is also not due to problems with gastrointestinal function or nutrition. The cause of this is because children with ichthyosis have increased caloric needs due to disruption of the skin barrier. Children with ichthyosis are also easier to lose air through the skin, this can overcome dehydration and constipation [18]. From the description above, the anamnesis results and physical examination support the case toward LI diagnosis.
LI differential diagnosis is Ichthyosis Vulgaris (IV). Ichthyosis vulgaris is a disorder as the result of filagrin gene mutation that works in keratinocyte differentiation. Ichthyosis vulgaris is characterized by xerosis, squama, pruritus also closely related to atopic condition. IV predilection is on extensor side of lower leg and back, with chest and stomach are rarely involved. IV manifestation appears at the age of 2 months and gets better during summer [10-12]. There was no symptom that support IV diagnosis in our patient, such as improvement during summer and xerosis upon certain body areas such as extensor side of leg and back.
Another differential diagnosis is ichthyosis linked to recessive chromosome X. Ichthyosis linked to recessive chromosome X is a genetic disorder generated by mutation in sulfatase steroid enzyme. Ichthyosis linked to recessive chromosome X also indicates overall scales at birth or shortly after birth. The scales are very much noticeable upon extremities, neck, torso, and buttocks. Flexural folds, palms, and soles are not scaly. The scales are often brown in color, strongly attached and separated by narrow area of skin which looks normal. Specific lesion related to the disease is the occurrence of asymptomatic corneal opacities [10-12]. In the case there was no irregular stromal corneal opacities and the scales cover all over body were not brown in color nor looked grubby, therefore differential diagnosis of recessive Ichthyosis linked to chromosome X was eliminated.
The feasible supporting examination to diagnose LI is histopathology examination and genetic analysis. Histopathology examination toward LI patient’s skin can discover the occurrence of hyperkeratosis with focal parakeratosis accompanied by hypergranulosis at the lower part [10]. It is in accordance with the histopathology examination in the case in which there was hyperkeratosis upon corneum stratum accompanied by focal parakeratosis and hypergranulosis. In genetic examination it can discover the occurrence of defect in gene 8 which is recognized as able to generate ARCI [1]. Genetic examination was not performed due to cost consideration and expensive instruments also it required special expertise to perform it.
LI management includes topical therapy, systemic therapy, and complication treatment. Topical therapy consists of moisturizer and topical keratolytic agent. The purpose is to improve the skin barrier function and facilitates desquamation. Furthermore, moisturizer can also serve to improve water binding capacity of corneum stratum [14]. The moisturizer applied can be in the form of urea, vitamin E acetate, glycerol and petroleum jelly. For patients with thick scales it is feasible to apply one or more keratolytic agents such as alpha-hydroxy acid, salicylic acid, N-acetylcysteine, urea (>5%) and glycol propylene [4,20].
Systemic management in the form of retinoid is a preference oral therapy for ichthyosis, especially for severe ichthyosis. Patients with LI are very much suited with retinoid application since retinoid can help the scales removal and prevent hyper proliferation. Retinoid application is suggested in a small dosage and it can be applied for a lifetime. The dosage of retinoid ranges from 1 mg/kgBW/day to 7 mg/kgWB/day [21,22]. Retinoid should be carefully applied and considering the side effect that may occur such as teratogen effect including malformation of central nerve system, cardiovascular, and it may cause spontaneous abortus as well as toxic side effect to the bones [5]. Therapy given in the case was in the form of Vaseline album smeared twice a day after bathing and olive oil as emollient smeared every 1-2 hours all over the body. Vaseline album is a moisturizer with occlusion effect that it can reduce Trans Eepidermal Water Loss (TEWL), whereas olive oil serves as emollient that is able to fill in the microscopic slits between keratinocytes [21]. Another therapy was gentamicin ointment which was smeared after applying NaCl 0,9% rub with gauze for 15 minutes, also the patient was suggested to bathe in pure cow milk of 1:10 liter once every 2-3 days. The result of consultation with ophthalmologist revealed the occurrence of sinistral and dextral ectropion which was treated with one drop of Cendo Lyteers 2-3 times a day to prevent keratitis and chloramphenicol cream was smeared onto eyelids to reduce eyelids stiffness. In the case patient was not given oral therapy due to age and side effect consideration that may occur as the result of oral retinoid. Besides it can also be added with keratinocyte modulator such as retinoid, calcipotriol and dexpanthenol.
The patient with LI is suggested to bathe every day since it facilitates the mechanic removal of the scales and it can maintain moisture. There is a suggestion to add natrium bicarbonate to denaturalize keratin and make water to be alkaline, that it is easier to remove the scales. Some other substances can be added to bath water, among others are rice starch, corn starch, and wheat starch [4]. Topical therapy includes moisturizer and topical keratolytic agent. We suggested our patient to milk bathe once every 2-3 days. The purpose is principally similar with the addition of various substances such as starch and wheat in order to make bathing liquid alkaline. The alkaline condition may facilitate the removal of the scales. The family was also educated related to the cause and course of the disease, since ichthyosis lamellar is a life time disease therefore the family’s participation and support both mentally and materially.
One of the recommended lifestyle changes is avoiding vigorous physical activity, because it can increase body temperature. This can worsen ichthyosis because it can lead to hypohidrosis thereby increasing the risk of heat stroke and seizures. Physiotherapy is also recommended to reduce contractures on flexion. Regular cleaning of the ear canal by an ENT-TOS specialist is also recommended to avoid hearing loss due to accumulation of scales in the ear canal [3,22,23]. IL patients have a normal age range, although the severe form rarely improves, causing psychological problems caused by cosmetic effects and depression and poor school performance. Therefore, family education, environment and lifelong therapy are needed to improve quality of life [5,24,25].
Conclusion
A case was reported of a boy aged 3 years and 11 months old with ichthyosis lamellar. The alloanamnesis revealed ailments of scaly skin just like fish scale, skin in eyes area was pulled backward and lips were pulled sideward. The family history did not indicate similar ailment. Physical examination discovered lamellar type squama with erythematosus base upon generalisata region generalisata, hyperkeratosis with a part of erosion and fissure upon bilateral palmar manus et plantar pedis region and tapered fingers was visible upon bilateral fingers region. Ectropion was visible upon bilateral okuli region, eclabium was visible upon oris region. The supporting examination revealed laboratory result was within normal limit, meanwhile histopathological examination by hematoxylin and eosin staining revealed there was focal hyperkeratosis upon hypergranulosis with mild psoriasiform hyperplasia upon epidermis layer also upon dermis layer it was visible that the papillary dermis, reticular and vascular dermis were within normal limit. The therapy given was in the form of topical treatment with Vaseline album and olive oil as the moisturizer, and bathing with water and milk mixture to remove the scales off the skin. The systemic therapy was not given due to side effect consideration that may obstruct patient’s growth. Patient experienced improvement although it was slow. A life time therapy is still required to improve the quality of life.
Conflict of Interests
The authors declare no conflicts of interest.
References
- Majmundar VD, Baxi K. Hereditary and acquired ichthyosis vulgaris. Treasure Island (FL): StatPearls Publishing. 2021 [Last accessed on October 06, 2021] https://www.ncbi.nlm.nih.gov/books/NBK562318/
- Louhichi N, Hadjsalem I, Marrakchi S, Trabelsi F, Masmoudi A, Turki H, et al. Congenital lamellar ichthyosis in Tunisia is caused by a founder nonsense mutation in the TGM1 gene. Mol Biol Rep. 2013;40(3):2527-32.
- Choate K, Milstone L. The Ichthyoses. In: Kang S, Amagai M, Bruckner A, Enk A, Margolis D, McMichael A, editors. Fitzpatrick’s dermatology. 9th New York: McGraw-Hill. 2019;775-815.
- Rodríguez-Pazos L, Ginarte M, Vega A, Toribio J. Autosomal recessive congenital ichthyosis. Actas Dermosifiliogr. 2013;104(4):270-84.
- Kurosawa M, Uehara R, Takagi A, Aoyama Y, Iwatsuki K, Amagai M, et al. Results of a nationwide epidemiologic survey of autosomal recessive congenital ichthyosis and ichthyosis syndromes in Japan. J Am Acad Dermatol. 2019;81(5):1086-92.
- Suraiyah S, Soedibyo S, Boediardja SA. Lamellar ichthyosis in a child with a history of infant collodion. Sari Pediat. 2016;9(1):32-8.
- Akiyama M. Corneocyte Lipid Envelope (CLE), the key structure for skin barrier function and ichthyosis pathogenesis. J Dermatol Sci. 2017;88(1):3-9.
- Cortés H, Magaña JJ, Reyes-Hernández OD, Zacaula-Juárez N, González-Torres M, Diaz-Beltrán W, et al. Non-invasive analysis of skin mechanical properties in patients with lamellar ichthyosis. Ski Res Technol. 2019;25(3):375-81.
- Parikh D. Lamellar ichtyosis-An update. Indian J Dermatol Vener Leprol. 2000;66(1):32-3.
- Takeichi T, Akiyama M. Inherited ichthyosis: Non-syndromic forms. J Dermatol. 2016;43(3):242-51.
- Vahlquist A, Fischer J, Törmä H. Inherited Nonsyndromic Ichthyoses: an update on pathophysiology, diagnosis and treatment. Am J Clin Dermatol. 2018;19(1):51-66.
- Crane J, Paller A. X-Linked Ichthyosis. Treasure Island (FL): StatPearls Publishing. 2021 [Last accessed on October 06, 2021] https://www.ncbi.nlm.nih.gov/books/NBK448149/
- Digiovanna JJ, Mauro T, Milstone LM, Schmuth M, Toro JR. Systemic retinoids in the management of ichthyoses and related skin types. Dermatol Ther. 2013;26(1):26-38.
- Aliyu I. Ocular Complications of lamellar Ichthyosis. Arch Med Heal Sci. 2018;6(1):134-5.
- Chakraborti C, Tripathi P, Bandopadhyay G, Mazumder D. Congenital bilateral ectropion in lamellar ichthyosis. Oman J Ophthalmol. 2011;4(1):35.
- Abboud JPJ, Whittington A, Ahmed M, Himebaugh JT, Wiley LA, Haffar A, et al. Apremilast Use in a Case of Cicatricial Ectropion Secondary to Severe Lamellar Ichthyosis. Ophthal Plast Reconstr Surg. 2018;34(3):e76-7.
- Al-Amry MA. Ocular manifestation of Ichthyosis. Saudi J Ophthalmol. 2016;30(1):39-43.
- Diaz LZ, Browning JC, Smidt AC, Rizzo WB, Levy ML. Complications of ichthyosis beyond the skin. Dermatol Ther. 2013;26(1):39-45.
- Sahay M, Sahay R. Rickets-vitamin D deficiency and dependency. Indian J Endocrinol Metab. 2012;16(2):164.
- Bassotti A, Moreno S, Criado E. Successful treatment with topical N-acetylcysteine in urea in five children with congenital lamellar ichthyosis. Pediatr Dermatol. 2011;28(4):451-5.
- Limmer A, Nwannunu C, Patel R, Mui U, Tyring S. Management of ichthyosis: a brief review. Ski Ther Lett. 2020;25(1):5-7.
- Zaenglein AL, Levy ML, Stefanko NS, Benjamin LT, Bruckner AL, Choate K, et al. Consensus recommendations for the use of retinoids in ichthyosis and other disorders of cornification in children and adolescents. Pediatr Dermatol. 2021;38(1):164-80.
- Taneja G, Dhanta A, Hazarika N. Response of short-term high-dose vitamin D therapy in lamellar ichthyosis: A rare case report. Dermatol Ther. 2020;33(6).
- Hanson B, Becker L, Hook K, Polcari I, Areaux RG, Maguiness S. Ectropion improvement with topical tazarotene in children with lamellar ichthyosis. Pediatr Dermatol. 2017;34(5):584-9.
- De Moraes ELL, Freire MH de S, Rocha F, Secco IL, Costa T, Afonso RQ. Nursing care for a newborn with Lamellar Ichthyosis: A case study in a neonatal unit. Rev da Esc Enferm. 2019;53:1-8.
This work is licensed under Attribution-NonCommercial-NoDerivs 2.0 Generic (CC BY-NC-ND 2.0) International License. With this license readers are free to share, copy and redistribute the material in any medium or format as long as the original source is properly cited.
Author Info
Adelia Wuri Pramudita1, Prasetyadi Mawardi1*
1Department of Dermatology and Venereology, Faculty of Medicine Sebelas Maret University, Dr. Moewardi General Hospital, Surakarta, Indonesia
*Corresponding Author: Prasetyadi Mawardi, Department of Dermatology and Venereology, Faculty of Medicine Sebelas Maret University, Dr. Moewardi General Hospital, Surakarta, Indonesia;
Email: prasetyadi_m@staff.uns.ac.id
Copyright
Copyright© 2021 by Mawardi P, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Citation: Mawardi P, et al. Lamelar Ichthyosis. Jour Clin Med Res. 2021;2(3) :1-11.

