Review Article | Vol. 3, Issue 2 | Journal of Clinical Medical Research | Open Access |
Prevalence of Hypertension in the Philippines in the Year 2050: Confronting a Major Challenge
Leilani B Mercado-Asis1,13,14*, Alberto A Atilano2,14, Deborah Ignacia D Ona3,14,15, Dolores D Bonzon4,14, Gilbert A Vilela5,14, Carlos L Chua6,14, Alejandro F Diaz7,14, Benjamin A Balmores Jr8,14, Esperanza I Cabral9,14, Abdias V Aquino10,14, Dante D Morales11,14, Nelson S Abelardo11,14, Lyn A Gomez12,14, Raymond V Oliva3,14, Rafael R Castillo11,13,14
1Section of Endocrinology and Metabolism, Department of Medicine, Faculty of Medicine and Surgery, University of Santo Toma, Manila, Philippines
2Department of Adult Cardiology, University of Santo Toma, Manila, Philippines
3Division of Hypertension, Department of Medicine, University of the Philippines College of Medicine, Manila, Philippines
4Department of Physiology, University of the Philippines College of Medicine, Manila, Philippines
5Department of Adult Cardiology, Philippine Heart Center, Quezon City, Philippines
6Section of Neurology, Department of Medicine, Manila Doctors Hospital, Manila, Philippines
7Section of Neuropsychiatry, Department of Medicine, University of Santo Tomas Hospital, Manila, Philippines
8Section of Nephrology, Department of Medicine, St. Luke’s Medical Center, Quezon City, Philippines
9Department of Adult Cardiology, Makati Medical Center, Makati City, Philippines
10Department of Neurology, St. Luke’s Medical Center, Quezon City, Philippines
11Department of Adult Cardiology, Manila Doctors Hospital, Manila, Philippines
12Department of Nephrology, Asian Hospital and Medical Center, Metro Manila, Philippines
13Cardio-Metabolic Research Unit (CaMeRU), FAME Leaders Academy, Makati City, Philippines
14Philippine Society of Hypertension, Philippines
15Department of Medicine, St. Luke’s Medical Center, Quezon City, Philippines
*Corresponding Author: Prof. Leilani B. Mercado-Asis, MD, PhD, MPH, MEd (DE), Address: Department of Medicine, Faculty of Medicine and Surgery, University of Santo Tomas, Manila, Philippines;
Email: lmasis@ust.edu.ph; medicalfiles.inquirer@gmail.com
Citation: Mercado-Asis LB, et al. Prevalence of Hypertension in the Philippines in the Year 2050: Confronting a Major Challenge. Jour Clin Med Res. 2022;3(2):1-13.
Copyright© 2022 by Mercado-Asis LB, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 18 Jul, 2022 | Accepted 06 Aug, 2022 | Published 13 Aug, 2022 |
Abstract
Background: The prevalence of hypertension in the Philippines has continuously increased in the past 22 years or more than two decades (from 1993 to 2015), with increased related deaths due to ischemic heart disease, stroke and chronic kidney disease.
Objective: The study aimed to project the prevalence of hypertension in the next three decades (by the year 2050) and the overall disease burden it may impose on the country.
Methods: We utilized data from the 2018 National Nutrition Survey (NNS) and the Philippine Statistical Authority (PSA) to project the prevalence of hypertension in the next three decades. A spline regression, which utilizes a non-linear regression technique, estimated the missing data sets in the hypertension prevalence by age and sex in a study conducted from 1993 to 2018. Factors predicting the share of deaths caused by hypertension included variables such as ischemic heart disease, stroke, chronic kidney disease and hypertensive heart disease. Post-hoc power analyses generated a large effect size (f2: 5.135) and high power (1.0) at an alpha level of 0.05.
Findings: Hypertension prevalence will remain high at 23%, with a 28% increase in the number of cases (24.28 million to 33.82 million) by 2050, given the population projection (101.60 million in 2015 to 142.10 million in 2050) and seriously affecting extremes of ages (the early 20s and 80s). In addition, actual number of deaths related to hypertension will increase more than double from 90,000 in 2015 to 210,000 due to ischemic heart disease, stroke and chronic kidney disease.
Interpretation: These findings demonstrate a significant increase in disease burden due to hypertension in the Philippines in the next three decades and possibly pose a significant public health challenge. Aggressive preventive and health-promoting efforts must be carried out to stem the tide of hypertensive cardiovascular disease in the country.
Keywords
Hypertension; Heart Disease; Strokes; Diabetes; Blood Pressure
Introduction
In the past four decades, the World Health Organization (WHO) reported a doubling in the number of affected individuals with Hypertension (HPN) or elevated Blood Pressure (BP) from 594 million to 1.13 billion, the majority of whom live in low- and middle-income countries [1]. With the increase in the aging population, prolonged life expectancy and continued rise in hypertension prevalence, the disease burden will significantly occur in the Asian region [2-5]. Globally, 51% of strokes and 45% of ischemic heart disease are attributable to uncontrolled blood pressure [3-4]. Most of the reports identified the determinants of hypertension in the male gender, obesity, smoking, unawareness of diabetes and hypercholesterolemia, low income, low educational attainment and urban dwelling [6-14].
For the past three decades (from 1993 to 2015), the hypertension prevalence in the Philippines based on the National Nutrition Survey conducted every five years showed a 21% to 25% increase [14,15]. However, with the country’s rapid population increase, the number of affected individuals with uncontrolled blood pressure continued to rise [14]. The velocity of increase will have a significant impact on the socioeconomic burden of the country. Awareness must be heightened for the community, governmental and non-governmental sectors to establish programs directed to curb the problem. With the preceding scenario, this study aims to project the prevalence of hypertension in the Philippines from 2020 to 2050. The findings will be essential to support call-to-action initiatives.
Methods
Preliminarily, we obtained the projected number of people in the Philippines from 2020 to 2050 classified by age (i.e., yearly age) and sex from published population data from the United Nations. The report estimated the population using expected fertility and net migration rates (United Nations World Population 2019) [16]. Subsequently, we determined the number of people with hypertension from 1998 to 2015 using data from the Food and Nutrition Research Institute’s (FNRI) National Nutrition Survey (NNS) [14]. The survey employed a stratified multi-stage sampling design, covering all regions and 79 provinces of the Philippines, conducted every five years from 1993 to 2008 and subsequently, every 2 to 3 years from 2008 to 2015.
In 2018 the survey became the Expanded National Nutrition Survey (ENNS) to address the need for local planning of specific and sensitive interventions [17]. The design included 37 to 40 provinces per year from 2018 to 2020, the grouping of which replicated rural and highly urbanized cities. These surveys assessed and reported anthropometry, biochemistry, diet, infant and young child feeding, maternal health and nutrition, food security program, socio-economic status and clinical health. Clinical anthropometrics include the prevalence of elevated blood pressure, high fasting blood glucose and dyslipidemia. Smoking, alcohol consumption, physical inactivity and an unhealthy diet were the behavioral risk factors that were assessed [17].
We utilized the data mentioned above to estimate the hypertension prevalence and cases by age group and gender from 1993 to 2018 using spline regression through SATA [17]. The resulting coefficients were then entered into a linear regression equation to predict hypertension cases from 2020 to 2050. The prevalence of hypertension from 2020 to 2050 was determined using the population report from UN (United Nations World Population 2019) data [16].
Further, the annual number of deaths attributed to hypertension was identified initially by estimating the number of deaths by age until 2050 using data from the Philippine Statistical Authority (PSA) [15]. Furthermore, we calculated the number of deaths due to hypertension by age group and gender using the Population Factor Attribution (PAF) for the Philippines from the Institute for Health Metrics and Evaluation (IHME) [18]. Factors predicting the share of deaths caused by hypertension included variables such as “ischemic heart disease, stroke, chronic kidney disease and hypertensive heart disease”. Finally, post-hoc power analyses generated a large effect size (f2: 5.135) and high power (1.0) at an alpha level of 0.05.
Results
Projection of Hypertension Prevalence by 2050 in the Philippines
For over two decades, the prevalence of hypertension among adults remained relatively stagnant, with a series of increases and decreases [14]. Following this long-term historical trend, the prevalence of hypertension in our projection study seems to have no significant change in the next 30 years (from 2015 to 2050), with 23.90% in 2015 and 23.80% in 2050 (Fig. 1) [15]. However, with a projected increase in the population from 101.60 million in 2015 to 142.10 million in 205015, Filipinos affected with hypertension will significantly increase from 24.28 million to 33.82 million. There is a higher prevalence growth among females, from 20.60% to 22.00% (Table 1).
Filipinos with hypertension among the adult population in our study will significantly increase from 2015 to 2050 with an overall ratio of 1.39 (Table 2). Hypertension prevalence will increase in the elderly individuals by two-folds, three-folds and more than five times among those in their 60s, 70s and 80s, respectively (Table 2). The young ones in their 20s will also be affected with hypertension manifesting earlier among the younger males.
Projection of Deaths and Cardiovascular Complications Due to Uncontrolled Hypertension by 2050
Hypertension-related deaths will increase by more than double, from an estimated 90,000 in 2015 to 210,000 in 2050. As presented in Fig. 2, the increase in hypertension-attributed deaths from 2015 to 2050 is due to the over-doubling of affected individuals: ischemic heart disease (35,000 to 82,000 cases), stroke (26,000 to 60,000 cases), hypertensive heart disease (17,000 to 40,000 cases) and chronic kidney disease 12,000 to 29,000 cases).
Projection of the Deceleration of Hypertension Prevalence in 2050 and its Effect on Cardiovascular Mortality
Using a 4.70% decline in the prevalence of hypertension, based on the 2018 ENNS result, the eventual prevalence of hypertension in the Philippines by 2050 will decrease to 15.60% (Fig. 3), providing a significant total reduction of 8.30% from 2015 [17]. The decrease in the prevalence was more observable among females (31.38%) than among males (17.00%). Moreover, a more significant decline in prevalence rate was noted in extreme age groups (the 20s to 30s and 60s to 80s) regardless of sex (Table 3). If deceleration continues until 2050, the projected mortality will decrease from 210,272 to 137,685. This decline will result in an estimated reduction of 72,587 deaths (Table 4).
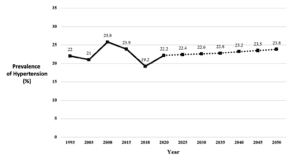
Figure 1: Rate of prevalence of elevated blood pressure (BP) among Filipino adults aged 20 years old and above, historical (years 1993 to 2015) and projected five-year interval from the years 2020 to 2050 using projection from historical years 1993 to 2015.
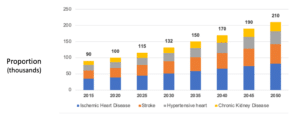
Figure 2: Projected number of deaths from various causes due to uncontrolled hypertension among adult Filipinos in 2015 (actual) and projected with five-year interval from years 2020 to 2050.
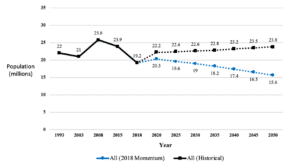
Figure 3: Projected decline in the prevalence of hypertension based on 2018 report versus 2015 report with projection to 2050.
Year 2015 | Year 2050 | |||
Prevalence Rate | Number of Filipino Adults with Hypertension (Millions) | Prevalence Rate | Number of Filipino Adults with Hypertension (Millions) | |
Male | 27.50% | 13.94 | 25.70% | 17.81 |
Female | 20.60% | 10.34 | 22.00% | 16.01 |
Total | 23.90% | 24.28 | 23.80% | 33.82 |
Table 1: Prevalence rate of elevated blood pressure and number of Filipino adults with hypertension in 2015 (actual) and in 2050 (projected using historical trend of 1993 to 2015).
Age group | Sex | Total | ||||||||||
Males | Females | |||||||||||
2015 | 2050 | 2015 | 2050 | 2015 (Actual) | 2050 (Projected) | Ratio (Projected 2050 vs. Actual 2015) | ||||||
Prevalence rate | Number of Filipino adults with hypertension (Millions) | Prevalence rate | Number of Filipino adults with hypertension (Millions) | Prevalence rate | Number of Filipino adults with hypertension (Millions) | Prevalence rate | Number of Filipino adults with hypertension (Millions) | Number of Filipino adults with hypertension (Millions) | ||||
20 – 24 Years Old | 12.40% | 1.15 | 8.70% | 0.66 | 3.00% | 0.26 | 1.00% | 0.07 | 1.41 | 0.73 | 0.52 | |
25 – 29 Years Old | 15.80% | 1.26 | 12.70% | 0.94 | 5.10% | 0.39 | 1.00% | 0.07 | 1.66 | 1.01 | 0.61 | |
30 – 34 Years Old | 19.60% | 1.38 | 17.30% | 1.23 | 8.50% | 0.58 | 3.80% | 0.26 | 1.96 | 1.49 | 0.76 | |
35 – 39 Years Old | 23.70% | 1.51 | 21.40% | 1.61 | 14.00% | 0.86 | 10.70% | 0.80 | 2.37 | 2.39 | 1.01 | |
40 – 44 Years Old | 28.10% | 1.58 | 25.10% | 1.78 | 21.00% | 1.16 | 14.50% | 1.01 | 2.73 | 2.79 | 1.02 | |
45 – 49 Years Old | 32.70% | 1.64 | 30.00% | 2.01 | 27.00% | 1.35 | 17.70% | 1.15 | 2.99 | 3.18 | 1.06 | |
50 – 54 Years Old | 37.00% | 1.56 | 35.50% | 2.23 | 31.10% | 1.31 | 22.30% | 1.40 | 2.88 | 3.63 | 1.26 | |
55 – 59 Years Old | 39.80% | 1.36 | 38.60% | 2.15 | 34.50% | 1.22 | 29.60% | 1.73 | 2.56 | 3.88 | 1.52 | |
60 – 64 Years Old | 40.90% | 1.02 | 38.50% | 1.72 | 37.90% | 1.03 | 39.20% | 1.94 | 2.05 | 3.62 | 1.77 | |
65 – 69 Years Old | 41.00% | 0.68 | 37.00% | 1.30 | 41.10% | 0.81 | 48.40% | 2.00 | 1.49 | 3.32 | 2.23 | |
70 – 74 Years Old | 40.80% | 0.41 | 35.60% | 0.95 | 43.40% | 0.58 | 55.30% | 1.92 | 0.98 | 2.87 | 2.94 | |
75 – 79 Years Old | 40.50% | 0.26 | 34.80% | 0.63 | 44.50% | 0.43 | 59.10% | 1.59 | 0.68 | 2.23 | 3.28 | |
≥80 Years Old | 39.60% | 0.17 | 35.60% | 0.59 | 42.50% | 0.36 | 58.20% | 2.07 | 0.53 | 2.67 | 5.06 | |
Total | 27.50% | 13.94 | 25.70% | 17.81 | 20.60% | 10.34 | 22.00% | 16.01 | 24.28 | 33.82 | 1.39 | |
Table 2: Number of Filipino adults with elevated blood pressure in 2015 (actual) and in 2050 (projected using historical trend of 1993 to 2015) according to age and sex.
Age Group | Sex | |||
Males | Females | |||
Historical trends up to 2015 | Historical trend using 2018 momentum | Historical trends up to 2015 | Historical trend using 2018 momentum | |
20 – 24 Years Old | -1.00% | -3.70% | 0.00% | 0.00% |
25 – 29 Years Old | -0.50% | -1.60% | -5.60% | -8.20% |
30 – 34 Years Old | -0.20% | -0.70% | -3.00% | -0.80% |
35 – 39 Years Old | -0.10% | -0.50% | -0.70% | -0.10% |
40 – 44 Years Old | -0.20% | -0.60% | -0.90% | -0.60% |
45 – 49 Years Old | -0.30% | -0.80% | -1.30% | -1.90% |
50 – 54 Years Old | -0.30% | -0.90% | -1.20% | -4.60% |
55 – 59 Years Old | -0.20% | -0.90% | -0.80% | -5.30% |
60 – 64 Years Old | -0.20% | -0.90% | -0.30% | -3.50% |
65 – 69 Years Old | -0.40% | -1.20% | 0.00% | -3.20% |
70 – 74 Years Old | -0.70% | -2.20% | 0.20% | -4.40% |
75 – 79 Years Old | -0.90% | -3.20% | 0.20% | -5.30% |
≥80 Years Old | -0.60% | -2.00% | 0.40% | -1.60% |
Table 3: Projected change of elevated blood pressure prevalence rates by sex and age segment using historical trend from 1993 to 2015 versus 2018 momentum.
Year | Number of deaths using historical trend projection | Number of deaths using 2018 momentum | Deaths Prevented |
2015 (Actual) | 90,208 | 90,208 | – |
2020 | 100,080 | 91,160 | (8,920) |
2025 | 115,168 | 101,042 | (14,126) |
2030 | 131,701 | 110,681 | (21,020) |
2035 | 149,999 | 119,476 | (30,523) |
2040 | 169,662 | 127,488 | (42,174) |
2045 | 190,127 | 133,697 | (56,430) |
2050 | 210,272 | 137,685 | (72,587) |
Table 4: Number of deaths attributed to hypertension among Filipino adults using historical trend projection from years 1993 to 2015 versus using projection with 2018 prevalence rate momentum.
Discussion
In the last two decades, the prevalence of hypertension in the Asian region seems to vary with an estimated range from 20% to 40%, with higher prevalence among urban dwellers regardless of socioeconomic status, conspicuously influenced by behavioral and metabolic factors such smoking, alcohol use, obesity and history of diabetes and hypercholesterolemia [6-14]. Low- to middle-income countries struggle to address significant morbidity and mortality due to uncontrolled blood pressure [19]. Regardless of economic status, the identified contributing factors to the burden of hypertension were low awareness, low percentage of the population on treatment and inadequate blood pressure control at a mere 50% and below [6-14,21,22].
In the Philippines, with the country’s increasing population, Filipinos with hypertension in the last two decades continued to increase from 8 million to 13 million [15]. Moreover, it will inflate to 33.82 million by 2050. In our study, a dramatic two- to six-fold increase will occur among the elderly, aged 65 to over 80 years, from 2% to 6.80%. This finding is congruent with data from other Asian countries owing to the aging population and longevity of life, foremost from India, China and Japan [2,6,10,22]. With a common finding of male preponderance, our study projects an increase in hypertensive individuals from 2015 to 2050 of 13.94 million to 17.81 million among males with a lesser number of 10.34 million to 16.01 million among females [2,6-10,22-25]. Behavioral factors like smoking and alcohol drinking could have caused the gender difference in hypertension prevalence [17].
The early development of hypertension among the younger population is another remarkable finding in our projection study. The male gender will be affected earlier than the female gender at 12.40% to 32.70% (20 to 49 years old) in 2015, with an average annual increase of 1.32% in 2050. Although young females will not have the same pattern, more will be affected as they age, with a prevalence of 39.20% to 59.10% at age 60 to 80. Overweight, obesity and physical inactivity are metabolic and behavioral risk factors becoming more prominent among young females. Females become more obese as they age [14,17].
Using a 4.70% decline in the prevalence of hypertension, the eventual prevalence in the Philippines in the year 2050 will decrease to 15.6%, providing a significant reduction of 8.30% from 2015 [17]. During the writing of our manuscript, the FNRI published the 2019 ENNS results [26]. An additional 1.70% decrease in the 2019 ENNS report resulted in a remarkable 9.0% total decrease in the prevalence of hypertension in four years (2015 to 2019) [26]. Only Singapore has attained such an early decline in hypertension prevalence at 7% (21.6% to 14.6%) among the Asian countries from 2000 to 2015 [27]. The other countries which showed a downward trend in hypertension prevalence were Korea and Japan [22,28]. The decrease in the prevalence of hypertension among Filipinos using the 2018 momentum will be more pronounced among females (31.38%) than among males (17.00%) in 2050. Moreover, there was a more significant decline in the prevalence rates in extreme age groups (the 20s to 30s and 60s to 80s) in males and female gender.
Robust programs and collaboration from governmental and non-governmental units seem to have contributed to the downward trend in hypertension in the Philippines [29-31]. Specifically, the 2012 Sin Tax Law was passed primarily to finance the Universal Health Care Program with a secondary objective of addressing public health issues related to alcohol and tobacco use [29]. Six years after its implementation, Austria and Pagaduan reported a significant reduction in annual cigarette consumption of households in all income brackets [32]. The 2018 and 2019 ENNS reports reflected this observation showing a decline in the proportion of smokers and alcohol drinkers in both genders, all age levels and in rural and urban dwellers, regardless of socioeconomic status [14,17].
Another effective health program is the 2012 Philippine Health Insurance Corporation (PhilHealth) Primary Care Benefits Package. Filipinos were able to avail of free out-patient screening for risk factors (diabetes, cholesterol) for hypertension in health units, which eventually expanded to out-patient availment of medications for hypertension [30]. This adaption enhanced this program by the Department of Health of the WHO Package of Essential (PEN) intervention program for non-communicable diseases to all its health units [31].
For the past 26 years, the Philippine Society of Hypertension (PSH), in collaboration with other related medical and non-medical organizations locally and internationally, has been active in its mission to address the hypertension problem through diagnosis, management and research. For over ten years, its partnership with the Department of Health has successfully increased public awareness through the 2009 Presidential Decree that made the month of May the “National Hypertension Awareness Month” through its established chapters all over the country. The month-long activities also highlight the World Hypertension Day (WHD) celebration of the World Health League of the International Society of Hypertension (ISH).
What could be considered the most significant achievement so far of PSH is the educational initiative of the society. Running on its 19th year, the Clinical Course in Hypertension Management Program has empowered over three thousand physicians and paramedical practitioners with hypertension’s basic and clinical knowledge. Over 500 physicians have been certified as hypertension specialists, now serving in the country’s far-flung areas. Through all these years, PSH has sustained its collaboration with other sectors like educators, media, lay and patients and legislators.
Lastly, the sustenance of effective programs is vital to achieving the targeted goal of reducing the prevalence of hypertension. All initiatives are geared toward halting the continuous increase in the morbidity and mortality rates due to adverse cardiovascular outcomes (ischemic heart disease, heart failure, stroke, chronic kidney disease), of which hypertension is a leading cause [1,19]. It was an eye-opener in this 2050 projection study that close to one hundred thousand deaths could be prevented and probably even more, if hypertension prevalence continuously declines.
Conclusion
The number of Filipinos afflicted with hypertension will continue to increase over the next three decades. As the prevalence of hypertension inflates, the disease burden due to chronic complications such as ischemic heart disease, stroke and chronic kidney disease will proportionally increase in the following years. These findings created a significant challenge for appropriate and timely intervention in all sectors.
Conflict of Interest
The authors declare no conflict of interest.
References
- Update by World Health Organization. Hypertension 2019. Last accessed on: August 05, 2022 https://www.who.int/news-room/fact-sheets/detail/hypertension
- Asian demographics. 2020. Last accessed on: August 05, 2022 https://www.worldometers.info/demographics/demographics-of-asia/
- World Health Organization. Global health observatory data repository. Raised blood pressure (SBP > 140 or DBP >, crude (%), estimates by country 2017. Last accessed on: August 05, 2022 https://apps.who.int/gho/data/view.main.2464EST?lang=en
- World Health Organization. Burden of disease: DALYs. 2004. Last accessed on: August 05, 2022 https://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_part4.pdf.
- The global economic burden of non-communicable diseases. 2011. Last accessed on: August 05, 2022 http://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf
- Man, REK, Gan AHW, Fenwick EK, Gan ATL, Gupta P, Sabanayagam C, et al. Prevalence, determinants and association of unawareness of diabetes, hypertension and hypercholesterolemia with poor disease control in a multi-ethnic Asian population without cardiovascular disease. Population Health Metrics. 2019;17:2-10.
- Kang SH, Kim SH, Cho JH, Yoon CH, Hwang SS, Lee HY, et al. Prevalence, awareness, treatment, and control of hypertension in Korea. J Hypertens. 2014;32(6):1170-7.
- Anchala R, Kannuri NK, Pant H, Khan H, Fraanco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hum Hypertens. 2017;32:66-74.
- Bhise, MD, Patra S. Prevalence and correlates of hypertension in Maharashtra, India: A multilevel analysis. Asia Pac J Public Health. 2019;31:101-12.
- Lu JL, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: Data from 1.7 million in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017:390:2549-58.
- Ahmed S, Tariqujjarman, Rahman A, Hasan Z, Hasan M. Inequalities in the prevalence of undiagnosed hypertension among Bangladesh adults: evidence from a nationwide survey. Indian Heart J. 2017;69:434-41.
- Majid NLA, Omar MA, Khoo YY, Naidu BM, Yn JLM, Hasani WSR, et al. Prevalence, awareness, treatment and control of hypertension in the Malaysian population: findings from the National Health and Morbidity Survey 2006-2015. J Hypertens. 2018:36:1680-8.
- Mehata S, Shrestha N, Mehta R, Vaidya A, Bahadur R, Bhattarai N, et al. Prevalence, awareness, treatment and control of hypertension in Nepal: data from nationally representative population-based cross-sectional study. Ann Glob Health. 2016;82:227-33.
- Food and Nutrition Research Institute. Last accessed on: August 05, 2022 https://www.fnri.dost.gov.ph/index.php/19-nutrition-statistic/175-national-nutrition-survey
- Philippine Statistics Authority. Philippine projection statistics. 2019. Last accessed on: August 05, 2022 https://psa.gov.ph/statistics/census/projected-population
- United Nations Department of Economic and Social Affairs. Population Dynamics. World Population Prospects 2019. Last accessed on: August 05, 2022 https://population.un.org/wpp/
- Food and Nutrition Research Institute. 2018 ENNS survey results presented during the 2019 National Nutrition Summit at Dusit Thani Manila. 2019. Last accessed on: August 05, 2022 https://www.fnri.dost.gov.ph/index.php/programs-and-projects/news-and-announcement/763-2018-expanded-national-nutrition-survey
- Institute for health metrics and evaluation. 2019. Last accessed on: August 05, 2022 https://vizhub.healthdata.org/gbd-compare/
- Chu D, Singh V. Obesity and hypertension in Asia: current sstatus and challenges. The Lancet Regional Health-Western Pacific. 2021;15:100243.
- Beany T, Schutte AE, Tomaszewski M, Ariti C, Burrell LM, Castillo RR, et al. FMED Sci on behalf of the MMM Investigators. May measurement month 2017: an analysis of blood pressure screening results worldwide. The Lancet Global Health. 2018;6:E736-43.
- Beany T, Burrell LM, Castillo RR, Charchar FJ, Cro S, Damasceno A, et al. May measurement month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur Heart J. 2019;40:2006-17.
- Hisamatsu T, Segawa H, Kadota A, Ohkubo T, Arima H, Miura K. Epidemiology of hypertension in Japan: beyond the new 2019 Japanese guidelines. Hypertens Res. 2020;43:1344-51.
- Jin CN, Yu CM, Sun JP, Fang F, Wen YN, Liu M. The healthcare burden of hypertension in Asia. Heart Asia 2013;5:238-243.
- Soenarta AA, Buranakitjaroen P, Chia YC, Chen CH, Nailes J, Hoshide S, et al. An overview of hypertension and cardiac involvement in Asia: Focus on heart failure. J Clin Hypertens. 2019;22(3):423-30.
- Cardiovascular diseases (CVDs). Update by World Health Organization. 2017. Last accessed on: August 05, 2022 https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- Food and Nutrition Research Institute. Expanded National Nutrition Survey (ENNS): 2019 results. Last accessed on: August 05, 2022 http://enutrition.fnri.dost.gov.ph/site/uploads/2019%20ENNS%20Provincial%20Dissemination%20-%20Angeles%20City.pdf
- Tay JCT, Teo BWT. Asian management of hypertension: current status, home blood pressure and specific concerns in Singapore. J Clin Hypertens. 2020;22:508-10.
- Kang SH, Kim SH, Cho JH, Yoon CH, Hwang SS, Lee HY, et al. Prevalence, awareness, treatment and control of hypertension in Korea. Sci Rep. 2019;9:10970.
- Republic Act No. 10351. The Sin Tax Law. 2012. Last accessed on: August 05, 2022 https://www.officialgazette.gov.ph/2012/12/19/republic-act-no-10351
- Philippine Health Insurance Corporation Circular No. 010. 2012. Last accessed on: August 05, 2022 https://www.philhealth.gov.ph/circulars/2012/circ10_2012.pdf
- Department of Health Administrative Order No. 2012-0029. 2012. Last accessed on: August 05, 2022 https://extranet.who.int/ncdccs/Data/PHL_D1_PHIL%20PEN.pdf
- Austria MS, Pagaduan JA. Assessing the impact of Philippine Sin Tax Reform Law on the demand of cigarettes. https://www.dlsu.edu.ph/wp-content/uploads/2019/03/aki_working_paper_no._2018-03-051.pdf
This work is licensed under Attribution-NonCommercial-NoDerivs 2.0 Generic (CC BY-NC-ND 2.0) International License. With this license readers are free to share, copy and redistribute the material in any medium or format as long as the original source is properly cited.
Author Info
Leilani B Mercado-Asis1,13,14*, Alberto A Atilano2,14, Deborah Ignacia D Ona3,14,15, Dolores D Bonzon4,14, Gilbert A Vilela5,14, Carlos L Chua6,14, Alejandro F Diaz7,14, Benjamin A Balmores Jr8,14, Esperanza I Cabral9,14, Abdias V Aquino10,14, Dante D Morales11,14, Nelson S Abelardo11,14, Lyn A Gomez12,14, Raymond V Oliva3,14, Rafael R Castillo11,13,14
1Section of Endocrinology and Metabolism, Department of Medicine, Faculty of Medicine and Surgery, University of Santo Toma, Manila, Philippines
2Department of Adult Cardiology, University of Santo Toma, Manila, Philippines
3Division of Hypertension, Department of Medicine, University of the Philippines College of Medicine, Manila, Philippines
4Department of Physiology, University of the Philippines College of Medicine, Manila, Philippines
5Department of Adult Cardiology, Philippine Heart Center, Quezon City, Philippines
6Section of Neurology, Department of Medicine, Manila Doctors Hospital, Manila, Philippines
7Section of Neuropsychiatry, Department of Medicine, University of Santo Tomas Hospital, Manila, Philippines
8Section of Nephrology, Department of Medicine, St. Luke’s Medical Center, Quezon City, Philippines
9Department of Adult Cardiology, Makati Medical Center, Makati City, Philippines
10Department of Neurology, St. Luke’s Medical Center, Quezon City, Philippines
11Department of Adult Cardiology, Manila Doctors Hospital, Manila, Philippines
12Department of Nephrology, Asian Hospital and Medical Center, Metro Manila, Philippines
13Cardio-Metabolic Research Unit (CaMeRU), FAME Leaders Academy, Makati City, Philippines
14Philippine Society of Hypertension, Philippines
15Department of Medicine, St. Luke’s Medical Center, Quezon City, Philippines
*Corresponding Author: Prof. Leilani B. Mercado-Asis, MD, PhD, MPH, MEd (DE), Address: Department of Medicine, Faculty of Medicine and Surgery, University of Santo Tomas, Manila, Philippines;
Email: lmasis@ust.edu.ph; medicalfiles.inquirer@gmail.com
Copyright
Copyright© 2022 by Mercado-Asis LB, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Citation: Mercado-Asis LB, et al. Prevalence of Hypertension in the Philippines in the Year 2050: Confronting a Major Challenge. Jour Clin Med Res. 2022;3(2):1-13.

