Case Report | Vol. 5, Issue 1 | Journal of Clinical Medical Research | Open Access |
Renal Limited Anti-Neutrophil Cytoplasmic Antibody Associated Vasculitis: A Case Report
Lydie Nengue1, Rameez Rao1, Viresh Monhanlal2, Valeria Cipolla Baumler1, Azeem Khan3, Steve J Carlan4*
1Department of Internal Medicine, USA
2Department of Nephrology, USA
3Department of Pathology, USA
4Division of Academic Affairs and Research, USA
*Correspondence author: Steve J Carlan, Division of Academic Affairs and Research, Orlando, Florida, USA; Email: stevecarlan@gmail.com
Citation: Carlan SJ, et al. Renal Limited Anti-Neutrophil Cytoplasmic Antibody Associated Vasculitis: A Case Report. Jour Clin Med Res. 2023;5(1):1-4.
Copyright© 2024 by Carlan SJ, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
| Received 25 Dec, 2023 | Accepted 15 Jan, 2024 | Published 22 Jan, 2024 |
Abstract
Background: Renal Limited Vasculitis (RLV) is a localized autoimmune vascular inflammatory disorder that is part of the Pauci Immune Glomerulonephritis (PIGN) spectrum. Over 90% of PIGN patients have circulating Anti-Neutrophil Cytoplasmic Antibodies (ANCA Ab). Anti-Neutrophil Cytoplasmic Antibody (ANCA) associated vasculitides are a heterogeneous group of multisystemic autoimmune disorders with distinct pathological findings. They are characterized by widespread inflammation of vessels according to their size, their location, and their serotypes based on the presence or absence of ANCA antibodies, namely Myeloperoxidase (MPO-ANCA), Proteinase-3 (PR3-ANCA) or simply ANCA negative, if no antibodies are found. RLV is characterized by antibody positivity to myeloperoxidase in the majority of cases.
Case Report: A 77-year-old Caucasian female was admitted with altered mental status and laboratory evidence of renal function compromise consistent with non-oliguric acute renal failure. Imaging and renal biopsy resulted in a diagnosis of pauci-immune glomerulonephritis consistent with MPO-ANCA vasculitis with a subtype that was associated with necrotizing arteritis, a severe form of the disease. She was placed on hemodialysis, intravenous cyclophosphamide, and oral prednisone, and entered remission.
Conclusion: A high level of suspicion and familiarity with clinical signs and symptoms are critical in distinguishing primary RPGN subtypes from other types of ANCA-associated small vessel vasculitis. If left untreated, renal limited vasculitis can progress to widespread systemic involvement and become fatal.
Keywords: ANCA Associated Vasculitis; Renal Limited Vasculitis; Rapidly Progressive Glomerulonephritis; Single Organ Vasculitis
Introduction
Pauci-Immune Glomerulonephritis (PIGN) is a necrotizing vasculitis of small vessels characterized by the absence or the paucity of immune complex deposits on Immunofluorescence (IF) or Electron Microscopy (EM). It is the most common variant of Rapidly Progressive Glomerulonephritis (RPG) which is a severe form of nephritic syndrome, which can progress to end-stage renal failure within a few days or weeks. Although constitutional signs and symptoms of systemic vasculitis are not seen in Renal Limited Vasculitis (RLV), elevated serum creatinine, hematuria, and proteinuria are very common. Thus, prompt diagnosis and treatment are warranted to improve the prognosis, especially in elderly patients.
Case Report
A 77-year-old Caucasian female with a past medical history of bladder cancer status post resection, hypertension, hyperlipidemia, and hypothyroidism, was admitted to our facility due to altered mental status. A day before admission, she was discharged from an outside hospital where she was treated for a urinary tract infection.
On admission, she had the following vital signs: HR 118, BP 152/52 mmHg height 157 cm; weight 66kg; temperature 36.6° with normal respiratory rate and saturation at room air. Physical examination findings were only relevant for bilateral 2+ pitting edema to the knees. Relevant laboratory workup was as follows: White Blood Cell (WBC) 19.5 (19.5 x 10⁹/L) without eosinophilia, serum creatinine 4.2 mg/dL (371.36 µmol/L), eGFR 25 (mL/min/1.73 m²), urea nitrogen 45 mg/dL (16.07 mmol/L), C-reactive protein 33.7 mg/dL, hemoglobin 6.5 g/dL and moderate electrolyte disturbances (Na 134 mEq/L, K 3.8 mEq/L, Cl 99 mmol/L, Ca 7.9 mg/dL). Her urinalysis showed WBC (5-10/HPF) and blood (250 RBC/uL). She also had proteinuria 178 mg/dL and an elevated urine protein/creatinine ratio of 2.7, with a normal C3 complement level (112 mg/dL). She had no family history of kidney disease prior to this admission.
The patient was originally diagnosed with non-oliguric acute renal failure, and placed on IV antibiotics and volume resuscitation. Given worsening renal condition despite treatment, nephrology was consulted and a kidney biopsy with ANCA panel was ordered. Other investigative workup included a chest X-ray, lumbar puncture, electroencephalogram, esophagogastroduodenoscopy, transthoracic echocardiogram, magnetic resonance imaging, and a computed tomogram of the abdomen and pelvis. They were all negative. A renal ultrasound was only relevant for right-sided calculus without hydronephrosis or obstructive uropathy.
The renal specimen showed severe necrotizing arteritis with transmural fibrinoid necrosis of the vessels (Fig. 1,2). Additionally, microscopic studies of the glomeruli revealed focal necrotizing glomerulonephritis without immune complex deposits, crescents, segmental sclerosis or endothelial tubuloreticular inclusions (Fig. 3). ANCA serology yielded anti Myeloperoxidase (MPO) antibody (p-ANCA > 8 EU). Anti-Proteinase 3 antibody (PR3) was negative. Furthermore, Antinuclear Antibody (ANA), anti-double stranded DNA (anti-dsDNA), complement levels, hepatitis and human immunodeficiency virus serologies, and anti-glomerular basement membrane diseases (anti-GBM diseases) were all negative. Her condition was diagnosed as pauci-immune glomerulonephritis consistent with MPO-ANCA vasculitis with a subtype that is associated with necrotizing arteritis, a severe form of the disease.
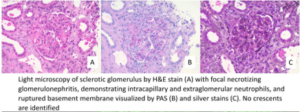
Figure 1: A-C: Light Microscopy specimen of glomeruli.
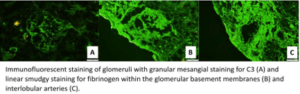
Figure 2: A-C: Immunofluorescence microscopy specimen of glomeruli.
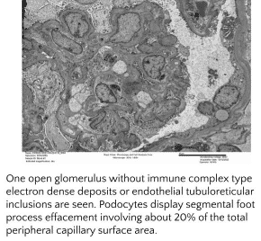
Figure 3: Electron Microscopy specimen of glomeruli.
Subsequently, she was placed on hemodialysis three times per week. She was put on induction therapy with IV pulse cyclophosphamide at 7.5 mg/kg every 3 weeks combined with daily oral prednisone 60 mg. She is currently on partial remission, with significant improvement of kidney function and negative MPO-ANCA titers.
Discussion
Pauci immune necrotizing glomerulonephritis is an immunopathological classification of rapidly progressive glomerulonephritis. It is usually part of a systemic vasculitis involving different organs simultaneously such as the ear-nose-throat, the lungs, the intestines or the kidneys. It is extremely rare to have instances where the inflammation is limited to the kidneys. In such cases, it is defined as Renal Limited Vasculitis. According to the amended version of the 1994 International Chapel Hill Consensus on the nomenclature of vasculitides, ANCA associated RLV should not be considered as a Single Organ Vasculitis (SOV) [1].
A kidney biopsy is required to establish a diagnosis and to differentiate among the different classes of primary RPGN [2]. A detailed history and examination should also be during the initial presentation. Recommended additional investigations include inflammatory markers, kidney function tests, and serological screening for diseases such as systemic lupus erythematosus and Goodpasture’s syndrome that should be considered in the differential diagnosis [3].
An ANCA antibody panel is important for classification, prognosis and response to treatment: patients with ANCA-positive glomerulonephritis that convert to ANCA-negative glomerulonephritis while undergoing treatment have a lower risk of relapses while high serum creatinine levels at presentation and dialysis-dependent renal failure correlate with a worse prognosis [4]. Besides, MPO-ANCA antibodies are quite frequent in RLV, accounting for the majority of cases. They are also encountered in microscopic polyangiitis. On the other hand, PR3-ANCA antibodies are associated with vasculitides of the respiratory tract such as granulomatosis with polyangiitis (Wegener), and eosinophilic granulomatosis with polyangiitis (Churg Strauss syndrome) [5]. Our case confirms these clinical findings but presents some atypical features.
Besides being encephalopathic on the first encounter, our patient didn’t have the classic crescent formation that is usually seen on biopsy of this type of RPGN. She was also reported to have severe necrotizing arteritis with transmural fibrinoid necrosis of small intrarenal arteries. This type of ANCA-Associated Vasculitis (AAV) usually affects older patients, with a more severe clinical presentation than patients without biopsy-proven arteritis, which suggests that it may be classified as a different subtype of AAV [6]. Worsening renal function requiring renal replacement therapy typically occurs within 3-6 months from initial presentation.
Currently, there is no standardized therapy for ANCA-associated RLV. The widely accepted protocol has two phases [7]. The induction phase, which varies between 3-6 months and consists of high-dose corticosteroids combined with cyclophosphamide, and the maintenance of remission phase, which is for relapse prevention. Our patient has achieved partial remission while in the induction phase, with a good prognosis [8].
Other therapeutic modalities such as rituximab and plasmapheresis could also be considered [9]. However, recent studies have shown that a rituximab-based treatment is not superior to conventional cyclophosphamide when used in the induction phase [10]. Therefore, using cyclophosphamide in this case was the best option according to the most recent clinical guidelines. Moreover, our case presented with necrotizing arteritis, which is a severe form of the disease. To the best of our knowledge, previous trials involving the use of rituximab did not include patients with necrotizing arteritis.
Conclusion
Renal-limited vasculitis is an exceedingly rare disease. It usually presents as RPGN. A high level of suspicion and familiarity with clinical signs and symptoms are critical in distinguishing primary RPGN subtypes from other types of ANCA-associated small vessel vasculitis with similar findings. Early diagnosis and prompt treatment with glucocorticoids and cyclophosphamide or rituximab remain effective in lowering mortality, especially in elderly patients. If left untreated, renal limited vasculitis can progress to widespread systemic involvement and become fatal. Severe necrotizing arteritis of the renal vessels is a very distinctive finding in this case.
Conflict of Interests
The authors have no conflict of interest to declare.
References
- Jennette JC. Overview of the 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Clin Exp Nephrol. 2013;17(5):603-6.
- Talon A, Tazi N. An Unusual presentation of pauci-immune necrotizing glomerulonephritis. Cureus. 2020;12(12):e12155.
- Yates M, Watts R. ANCA-associated vasculitis. Clin Med (Lond). 2017;17(1):60-4.
- Jennette JC, Nachman PH. ANCA Glomerulonephritis and vasculitis. Clin J Am Soc Nephrol. 2017;12(10):1680-91.
- Syed R, Rehman A, Valecha G, El-Sayegh S. Pauci-immune crescentic glomerulonephritis: An ANCA-Associated Vasculitis. Biomed Res Int. 2015;2015:402826.
- Boudhabhay I, Delestre F, Coutance G, Gnemmi V, Quemeneur T, Vandenbussche C, et al. Reappraisal of renal arteritis in ANCA-associated vasculitis: clinical characteristics, pathology, and outcome. J Am Soc Nephrol. 2021;32(9):2362-74.
- Rutgers A, Sanders JS, Stegeman CA, Kallenberg CG. Pauci-immune necrotizing glomerulonephritis. Rheum Dis Clin North Am. 2010;36(3):559-72.
- Turkmen K, Ozer H, Tesar V. An update on dıagnosıs and treatment of ANCA associated renal vasculıtıs. Int Urol Nephrol. 2023;55(11):2817-27.
- Jones RB, Cohen Tervaert JW, Hauser T, Luqmani R, Morgan MD, Peh CA, et. al. Rituximab versus cyclophosphamide in ANCA-associated renal vasculitis. N Engl J Med. 2010;363(3):211-20.
- Watts RA, Robson J. Introduction, epidemiology and classification of vasculitis. Best Pract Res Clin Rheumatol. 2018;32(1):3-20.
This work is licensed under a Creative Commons Attribution 2.0 International License.
Author Info
Lydie Nengue1, Rameez Rao1, Viresh Monhanlal2, Valeria Cipolla Baumler1, Azeem Khan3, Steve J Carlan4*
1Department of Internal Medicine, USA
2Department of Nephrology, USA
3Department of Pathology, USA
4Division of Academic Affairs and Research, USA
*Correspondence author: Steve J Carlan, Division of Academic Affairs and Research, Orlando, Florida, USA; Email: stevecarlan@gmail.com
Copyright
Copyright© 2024 by Carlan SJ, et al. All rights reserved. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation
Citation: Carlan SJ, et al. Renal Limited Anti-Neutrophil Cytoplasmic Antibody Associated Vasculitis: A Case Report. Jour Clin Med Res. 2023;5(1):1-4.

